Sunday Poster Session
Category: Colorectal Cancer Prevention
P0443 - A Prospective Study of Depth of Colonoscope Insertion and Adenoma Detection Rate
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Joy Yates, DO
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Joy Yates, DO1, Sarah Wehbe, MD2, Qijun Yang, MS2, Jessica Crimaldi, NP2, Carol A.. Burke, MD, FACG3
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH; 3Digestive Disease Institute, Cleveland Clinic, Cleveland, OH
Introduction: High adenoma detection rate (ADR) reduces colorectal cancer incidence and mortality. Patient, endoscopist, and procedural factors are associated with ADR. However other technical aspects of colonoscopy performance such as depth of scope insertion (DOI) upon reaching the cecum has not been studied. We hypothesized a lower DOI, suggesting loop reduction on insertion would be associated with greater mucosal exposure on withdrawal, and thus an increase in ADR. Our aim was to assess DOI and its impact on ADR.
Methods: An IRB approved prospective study of consecutive consenting patients undergoing outpatient colonoscopy from March 2024-May 2024 was performed. Patients with incomplete exams, inadequate bowel preparation, prior colonic surgery, IBD, and hereditary colorectal cancer syndromes were excluded. Clinical factors, endoscopist and procedural details including DOI were obtained. Regression analysis was performed to identify predictors of DOI and ADR.
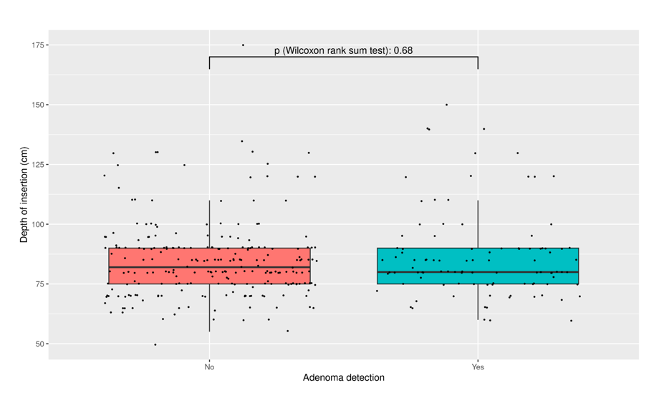
Results: 329 patients with a median age of 58 years of whom 53.2% female were included (Table 1). 76% of exams were for screening or surveillance. ADR was 34.6% for males and 27% for females. DOI ranged from 50 cm-175 cm. The median DOI was 82.0 cm [IQR 75.0;90.0] versus 80 cm [IQR 75.0;90.0] for patients without and with adenomas (Figure 1, p = 0.68). Compared to DOI of ≤ 75 cm, a DOI of 76-81 cm had highest ADR, followed by 82-90 cm, and ≥ 91 cm (OR 1.46, 1.09, and 1.06 respectively, p = NS). Three factors were significantly associated with average DOI: every unit increase in BMI kg/m² increased DOI by 0.71 cm and each additional year from terminal training of the endoscopist increased DOI by 0.21 cm. Female endoscopists were associated with a 5.8 cm lower DOI when compared to male endoscopists. Patient age, sex, prior abdominal surgery, endoscopist’s specialty, sedation type, bowel preparation, perceived procedure difficulty and patient tolerance were not significantly related to DOI.
Discussion: In this small prospective study, there was a trend for lower DOI and higher ADR. The lack of statistical significance may be due to type II error. Enrollment will continue and further analyses will also include assessment of number of adenomas per colonoscopy.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joy Yates, DO1, Sarah Wehbe, MD2, Qijun Yang, MS2, Jessica Crimaldi, NP2, Carol A.. Burke, MD, FACG3. P0443 - A Prospective Study of Depth of Colonoscope Insertion and Adenoma Detection Rate, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH; 3Digestive Disease Institute, Cleveland Clinic, Cleveland, OH
Introduction: High adenoma detection rate (ADR) reduces colorectal cancer incidence and mortality. Patient, endoscopist, and procedural factors are associated with ADR. However other technical aspects of colonoscopy performance such as depth of scope insertion (DOI) upon reaching the cecum has not been studied. We hypothesized a lower DOI, suggesting loop reduction on insertion would be associated with greater mucosal exposure on withdrawal, and thus an increase in ADR. Our aim was to assess DOI and its impact on ADR.
Methods: An IRB approved prospective study of consecutive consenting patients undergoing outpatient colonoscopy from March 2024-May 2024 was performed. Patients with incomplete exams, inadequate bowel preparation, prior colonic surgery, IBD, and hereditary colorectal cancer syndromes were excluded. Clinical factors, endoscopist and procedural details including DOI were obtained. Regression analysis was performed to identify predictors of DOI and ADR.
Results: 329 patients with a median age of 58 years of whom 53.2% female were included (Table 1). 76% of exams were for screening or surveillance. ADR was 34.6% for males and 27% for females. DOI ranged from 50 cm-175 cm. The median DOI was 82.0 cm [IQR 75.0;90.0] versus 80 cm [IQR 75.0;90.0] for patients without and with adenomas (Figure 1, p = 0.68). Compared to DOI of ≤ 75 cm, a DOI of 76-81 cm had highest ADR, followed by 82-90 cm, and ≥ 91 cm (OR 1.46, 1.09, and 1.06 respectively, p = NS). Three factors were significantly associated with average DOI: every unit increase in BMI kg/m² increased DOI by 0.71 cm and each additional year from terminal training of the endoscopist increased DOI by 0.21 cm. Female endoscopists were associated with a 5.8 cm lower DOI when compared to male endoscopists. Patient age, sex, prior abdominal surgery, endoscopist’s specialty, sedation type, bowel preparation, perceived procedure difficulty and patient tolerance were not significantly related to DOI.
Discussion: In this small prospective study, there was a trend for lower DOI and higher ADR. The lack of statistical significance may be due to type II error. Enrollment will continue and further analyses will also include assessment of number of adenomas per colonoscopy.
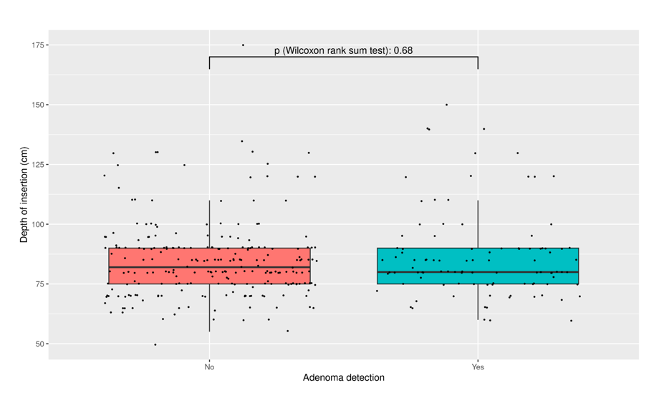
Figure: Figure 1. Depth of insertion and Adenoma Detection
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Joy Yates indicated no relevant financial relationships.
Sarah Wehbe indicated no relevant financial relationships.
Qijun Yang indicated no relevant financial relationships.
Jessica Crimaldi indicated no relevant financial relationships.
Carol Burke: Abbvie – Other. Ambry Genetics – Speakers Bureau. Emtora Biosciences – Grant/Research Support. Guardant – Consultant. Lumabridge – Consultant. Medtronic – Other. Myriad – Other. Sebela – Consultant.
Joy Yates, DO1, Sarah Wehbe, MD2, Qijun Yang, MS2, Jessica Crimaldi, NP2, Carol A.. Burke, MD, FACG3. P0443 - A Prospective Study of Depth of Colonoscope Insertion and Adenoma Detection Rate, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
