Sunday Poster Session
Category: Colorectal Cancer Prevention
P0447 - Ceiling Effect of CADe in Improving Detection Rates in FIT Positive Cases Among Gastroenterologists With High Baseline ADR
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- HS
Hussam Sabbagh, MD
Wayne State University School of Medicine / Detroit Medical Center
Detroit, MI
Presenting Author(s)
Hussam Sabbagh, MD1, Tooba Tariq, MD1, TJ Wilson, MD1, Ziad Kanaan, MD, PhD2, Kirthi Lilley, MD2, Samara Rifkin, MD2, Fadi Antaki, MD3
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2John D. Dingell VA Medical Center, Detroit, MI; 3John D. Dingell VA Medical Center and Wayne State University School of Medicine, Detroit, MI
Introduction: Artificial intelligence (AI) devices have been shown to increase adenoma detection rate (ADR) during screening colonoscopy in randomized controlled trials. The real-life data has been inconsistent. There is a paucity of data about the incremental benefit of AI when the baseline ADR is elevated. Patients who undergo colonoscopy for the evaluation of a positive fecal immunochemical test (FIT) for occult blood have increased prevalence of colorectal neoplasia. In this study, we compare adenoma detection rates (ADR) in FIT positive patients before and after the introduction of computer aided detection devices (CADe) (GI Genius, Medtronic) at an academic Veterans Affairs medical center.
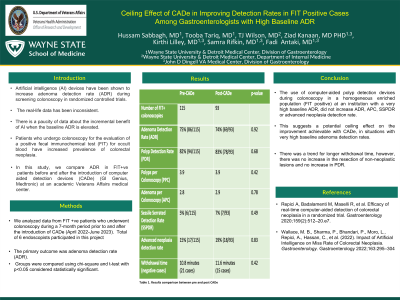
Methods: We analyzed data from FIT positive patients who underwent colonoscopy during a 7-month period prior to and after the introduction of CADe (April 2022-June 2023). The primary outcome was adenoma detection rate (ADR). Secondary outcomes included polyp detection rate (PDR), average number of polyps per colonoscopy (PPC), average number of adenomas per colonoscopy (APC), sessile serrated polyp detection rate (SSPDR), advanced neoplasm detection rate, and withdrawal time (in cases without intervention). Groups were compared using chi-square and t-test with p< 0.05 considered statistically significant.
Results: A total of 208 colonoscopies were performed for positive FIT (115 pre-CADe and 93 post-CADe). ADR was 75% vs. 74% (p=0.92), PDR was 82% vs. 83% (p=0.68), PPC was 3.9 vs. 3.9 (p=0.42), APC was 2.8 vs. 2.9 (p=0.78), SSPDR was 5% vs. 8% (p=0.49), and advanced neoplasia detection rate was 15% vs. 19% (p=0.83), respectively. Colonoscopy without intervention was performed in 21 cases in the pre-CADe group and 15 cases in the post-CADe group. In those procedures, withdrawal time was 10.8 minutes vs. 11.6 minutes (p=0.42), respectively.
Discussion: The use of computer-aided polyp detection devices during colonoscopy in a homogeneous enriched population (FIT positive) at an institution with a very high baseline ADR, did not increase ADR, APC, SSPDR or advanced neoplasia detection rate. There was a trend for longer withdrawal time, however, there was no increase in the resection of non-neoplastic lesions and no increase in PDR. This suggests a potential ceiling effect on the improvement achievable with CADe, in situations with very high baseline adenoma detection rates.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hussam Sabbagh, MD1, Tooba Tariq, MD1, TJ Wilson, MD1, Ziad Kanaan, MD, PhD2, Kirthi Lilley, MD2, Samara Rifkin, MD2, Fadi Antaki, MD3. P0447 - Ceiling Effect of CADe in Improving Detection Rates in FIT Positive Cases Among Gastroenterologists With High Baseline ADR, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2John D. Dingell VA Medical Center, Detroit, MI; 3John D. Dingell VA Medical Center and Wayne State University School of Medicine, Detroit, MI
Introduction: Artificial intelligence (AI) devices have been shown to increase adenoma detection rate (ADR) during screening colonoscopy in randomized controlled trials. The real-life data has been inconsistent. There is a paucity of data about the incremental benefit of AI when the baseline ADR is elevated. Patients who undergo colonoscopy for the evaluation of a positive fecal immunochemical test (FIT) for occult blood have increased prevalence of colorectal neoplasia. In this study, we compare adenoma detection rates (ADR) in FIT positive patients before and after the introduction of computer aided detection devices (CADe) (GI Genius, Medtronic) at an academic Veterans Affairs medical center.
Methods: We analyzed data from FIT positive patients who underwent colonoscopy during a 7-month period prior to and after the introduction of CADe (April 2022-June 2023). The primary outcome was adenoma detection rate (ADR). Secondary outcomes included polyp detection rate (PDR), average number of polyps per colonoscopy (PPC), average number of adenomas per colonoscopy (APC), sessile serrated polyp detection rate (SSPDR), advanced neoplasm detection rate, and withdrawal time (in cases without intervention). Groups were compared using chi-square and t-test with p< 0.05 considered statistically significant.
Results: A total of 208 colonoscopies were performed for positive FIT (115 pre-CADe and 93 post-CADe). ADR was 75% vs. 74% (p=0.92), PDR was 82% vs. 83% (p=0.68), PPC was 3.9 vs. 3.9 (p=0.42), APC was 2.8 vs. 2.9 (p=0.78), SSPDR was 5% vs. 8% (p=0.49), and advanced neoplasia detection rate was 15% vs. 19% (p=0.83), respectively. Colonoscopy without intervention was performed in 21 cases in the pre-CADe group and 15 cases in the post-CADe group. In those procedures, withdrawal time was 10.8 minutes vs. 11.6 minutes (p=0.42), respectively.
Discussion: The use of computer-aided polyp detection devices during colonoscopy in a homogeneous enriched population (FIT positive) at an institution with a very high baseline ADR, did not increase ADR, APC, SSPDR or advanced neoplasia detection rate. There was a trend for longer withdrawal time, however, there was no increase in the resection of non-neoplastic lesions and no increase in PDR. This suggests a potential ceiling effect on the improvement achievable with CADe, in situations with very high baseline adenoma detection rates.
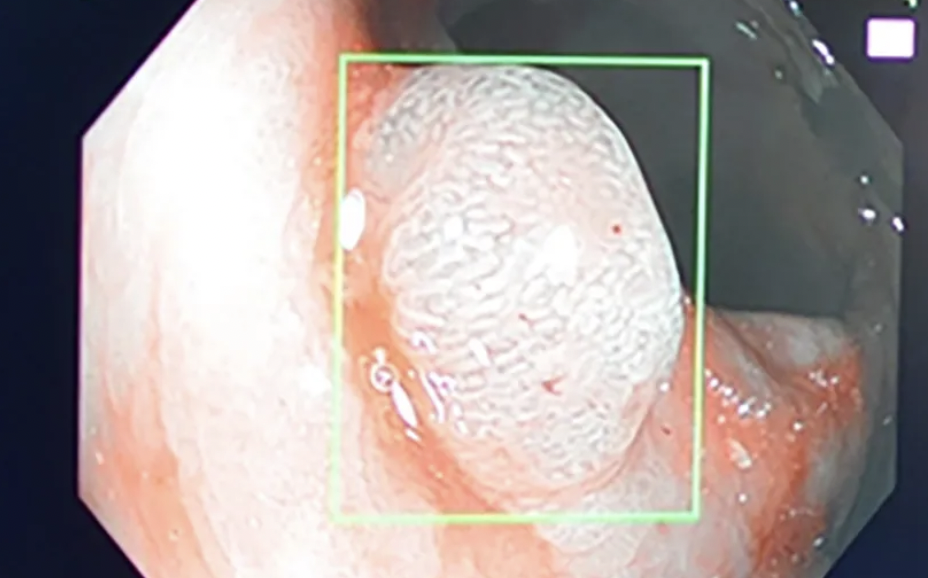
Figure: Polyp Detection by AI in Colonoscopy
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Hussam Sabbagh indicated no relevant financial relationships.
Tooba Tariq indicated no relevant financial relationships.
TJ Wilson indicated no relevant financial relationships.
Ziad Kanaan indicated no relevant financial relationships.
Kirthi Lilley indicated no relevant financial relationships.
Samara Rifkin indicated no relevant financial relationships.
Fadi Antaki indicated no relevant financial relationships.
Hussam Sabbagh, MD1, Tooba Tariq, MD1, TJ Wilson, MD1, Ziad Kanaan, MD, PhD2, Kirthi Lilley, MD2, Samara Rifkin, MD2, Fadi Antaki, MD3. P0447 - Ceiling Effect of CADe in Improving Detection Rates in FIT Positive Cases Among Gastroenterologists With High Baseline ADR, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

