Sunday Poster Session
Category: Esophagus
P0484 - PPI Stewardship: A Quality Improvement Tool to Improve Long-Term Prescribing Practices
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- JS
Jessica Sosio, DO
Indiana University School of Medicine
Evansville, IN
Presenting Author(s)
Jessica Sosio, DO1, Niamh McKee, MB1, Robert Gold, PhD. MBA2, Adrian Singson, MD3, Konstantin Boroda, MD4
1Indiana University School of Medicine, Evansville, IN; 2Ascension St. Vincent, Evansville, IN; 3Indiana University School of Medicine, Vincennes, IN; 4Indiana University School of Medicine/Ascension St. Vincent, Evansville, IN
Introduction: Proton pump inhibitors (PPIs) are the third most sold drug in the United States. Overuse has been linked to adverse events including osteoporotic fractures and kidney disease. Per American Gastroenterological Association (AGA) Practice Guidance, long-term PPI (LTPPI) use is warranted in Barrett’s esophagus, clinically significant (LA Classification grade C/D) erosive esophagitis, esophageal strictures from gastroesophageal reflux disease (GERD), Zollinger-Ellison syndrome, eosinophilic esophagitis, and gastroprotection in users of aspirin/nonsteroidal anti-inflammatory drugs at high risk for gastrointestinal bleeding. Overprescription also imposes an economic cost and contributes to polypharmacy, especially in the elderly. Therefore, de-prescribing is important.
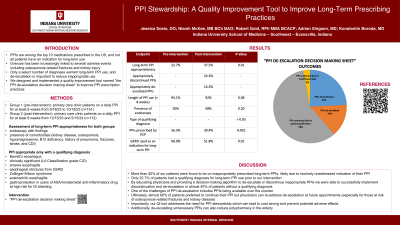
Methods: LTPPI appropriateness was assessed in our primary care clinic among patients on daily PPI for at least 8 weeks between 9/18/23 and 10/18/23 (pre-intervention group, n=151). Endoscopic findings and presence of comorbidities (kidney disease, osteoporosis, hypomagnesemia, B12 deficiency, history of pneumonia, fractures, stroke, and C. difficile infection) were noted. Appropriateness was based on the 2022 AGA Practice Guidance. From 12/15/23 to 5/15/24, a “PPI de-escalation decision making sheet” was distributed by the pharmacist to the physicians for guidance on LTPPI continuation or deprescription (post-intervention group, n=112).
Results: There was a significant difference in LTPPI appropriateness (p 0.01), 22.7% and 37.5% pre- and post-intervention. With intervention, 24.3% of PPIs were discontinued, 14.3% de-escalated, 2.8% continued due to insufficient data, and 58.6% continued per patient preference. No difference was found for PPI length of use and dose, presence of endoscopy, and qualifying diagnosis. Pre-intervention, primary care providers prescribed LTPPIs significantly more (p 0.001), and GERD was used as an indication (p 0.01). Regarding comorbidities, only differences in kidney disease (p 0.04) pre-intervention and fractures (p 0.04) post-intervention were found.
Discussion: Successful LTPPI de-prescription plays a role in minimizing risk of adverse events. By providing a list of qualifying diagnoses and an algorithm to de-escalate LTPPIs, we made a significant impact on PPI deprescription. Comorbidities were not used as part of the decision-making process but were noted to highlight that patients already at risk were being prescribed LTPPIs. Therefore, they were not considered confounding variables.
Disclosures:
Jessica Sosio, DO1, Niamh McKee, MB1, Robert Gold, PhD. MBA2, Adrian Singson, MD3, Konstantin Boroda, MD4. P0484 - PPI Stewardship: A Quality Improvement Tool to Improve Long-Term Prescribing Practices, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Indiana University School of Medicine, Evansville, IN; 2Ascension St. Vincent, Evansville, IN; 3Indiana University School of Medicine, Vincennes, IN; 4Indiana University School of Medicine/Ascension St. Vincent, Evansville, IN
Introduction: Proton pump inhibitors (PPIs) are the third most sold drug in the United States. Overuse has been linked to adverse events including osteoporotic fractures and kidney disease. Per American Gastroenterological Association (AGA) Practice Guidance, long-term PPI (LTPPI) use is warranted in Barrett’s esophagus, clinically significant (LA Classification grade C/D) erosive esophagitis, esophageal strictures from gastroesophageal reflux disease (GERD), Zollinger-Ellison syndrome, eosinophilic esophagitis, and gastroprotection in users of aspirin/nonsteroidal anti-inflammatory drugs at high risk for gastrointestinal bleeding. Overprescription also imposes an economic cost and contributes to polypharmacy, especially in the elderly. Therefore, de-prescribing is important.
Methods: LTPPI appropriateness was assessed in our primary care clinic among patients on daily PPI for at least 8 weeks between 9/18/23 and 10/18/23 (pre-intervention group, n=151). Endoscopic findings and presence of comorbidities (kidney disease, osteoporosis, hypomagnesemia, B12 deficiency, history of pneumonia, fractures, stroke, and C. difficile infection) were noted. Appropriateness was based on the 2022 AGA Practice Guidance. From 12/15/23 to 5/15/24, a “PPI de-escalation decision making sheet” was distributed by the pharmacist to the physicians for guidance on LTPPI continuation or deprescription (post-intervention group, n=112).
Results: There was a significant difference in LTPPI appropriateness (p 0.01), 22.7% and 37.5% pre- and post-intervention. With intervention, 24.3% of PPIs were discontinued, 14.3% de-escalated, 2.8% continued due to insufficient data, and 58.6% continued per patient preference. No difference was found for PPI length of use and dose, presence of endoscopy, and qualifying diagnosis. Pre-intervention, primary care providers prescribed LTPPIs significantly more (p 0.001), and GERD was used as an indication (p 0.01). Regarding comorbidities, only differences in kidney disease (p 0.04) pre-intervention and fractures (p 0.04) post-intervention were found.
Discussion: Successful LTPPI de-prescription plays a role in minimizing risk of adverse events. By providing a list of qualifying diagnoses and an algorithm to de-escalate LTPPIs, we made a significant impact on PPI deprescription. Comorbidities were not used as part of the decision-making process but were noted to highlight that patients already at risk were being prescribed LTPPIs. Therefore, they were not considered confounding variables.
Disclosures:
Jessica Sosio indicated no relevant financial relationships.
Niamh McKee indicated no relevant financial relationships.
Robert Gold indicated no relevant financial relationships.
Adrian Singson indicated no relevant financial relationships.
Konstantin Boroda indicated no relevant financial relationships.
Jessica Sosio, DO1, Niamh McKee, MB1, Robert Gold, PhD. MBA2, Adrian Singson, MD3, Konstantin Boroda, MD4. P0484 - PPI Stewardship: A Quality Improvement Tool to Improve Long-Term Prescribing Practices, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
