Sunday Poster Session
Category: Esophagus
P0487 - Exploring Demographic Variations in Eosinophilic Esophagitis: A Nationwide Study of Hospital Admissions From 2019-2023
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
- RR
Rajmohan Rammohan, MD
Nassau University Medical Center
East Meadow, NY
Presenting Author(s)
Raj Mohan Ram Mohan, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Leeza Pannikodu, MD, Winghang Lau, MD, Abhishek Tadikonda, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Paul Mustacchia, MD, MBA
Nassau University Medical Center, East Meadow, NY
Introduction: Eosinophilic esophagitis (EoE) is an inflammatory condition that varies widely in incidence across different racial and gender groups. This study examines how race and gender influence the prevalence of EoE, exploring patterns and disparities. The research aims to identify which groups are most at risk through detailed statistical analysis, thereby informing targeted medical interventions and increasing awareness of the demographic variations in this chronic disease.
Methods: Data from the Nationwide Admission Database (HCUP) for 2019-2023 on 1,748,576 adult hospital admissions with a primary diagnosis of Eosinophilic esophagitis was analyzed. The study began with an inspection of the dataset's structure, emphasizing race, gender, and eosinophilic esophagitis indicators. Incidence rates were summarized by demographics, followed by chi-square tests to identify significant incidence variations among different racial and gender groups, using contingency tables for statistics and p-values. Logistic regression was then applied to further explore these associations, with race and gender as predictors, and eosinophilic esophagitis as the dependent outcome
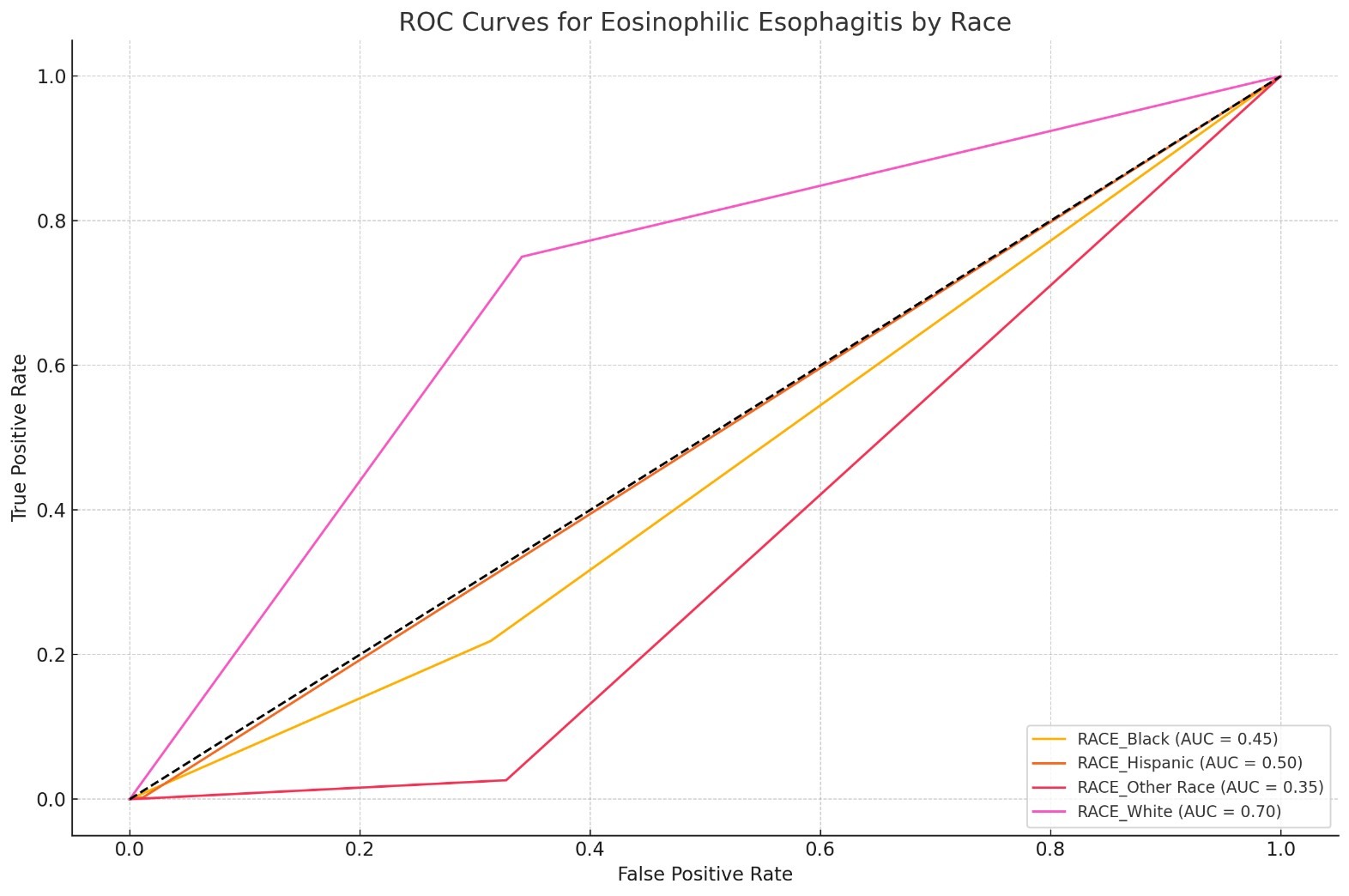
Results: Between 2019 and 2023, 1,748,576 patients were admitted; 11051 Eosinophilic esophagitis patients were studied after propensity score matching. Logistic regression analysis highlights significant racial and gender disparities in eosinophilic esophagitis incidence. White individuals have the highest likelihood (coefficient: 2.2411, p< 0.0001), with Blacks also at increased risk (coefficient: 1.0911, p< 0.0001). Conversely, Other Races have a reduced likelihood (coefficient: -1.0702, p< 0.0001). No significant odds difference is seen in Hispanics (coefficient: -0.0102, p=0.9742). Males are less likely to develop the condition than females (coefficient: -0.1760, p< 0.0001), emphasizing race and gender's role in the disease's prevalence.
Discussion: The study highlights significant racial and gender disparities in eosinophilic esophagitis (EoE) incidence, emphasizing the need for tailored healthcare strategies. Increased prevalence among White and Black populations suggests potential genetic or environmental influences, while the higher incidence in females may indicate hormonal or immune variations. These findings support the development of customized medical approaches that consider these demographic factors to improve treatment outcomes and efficacy in EoE managemen
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Raj Mohan Ram Mohan, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Leeza Pannikodu, MD, Winghang Lau, MD, Abhishek Tadikonda, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Paul Mustacchia, MD, MBA. P0487 - Exploring Demographic Variations in Eosinophilic Esophagitis: A Nationwide Study of Hospital Admissions From 2019-2023, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Nassau University Medical Center, East Meadow, NY
Introduction: Eosinophilic esophagitis (EoE) is an inflammatory condition that varies widely in incidence across different racial and gender groups. This study examines how race and gender influence the prevalence of EoE, exploring patterns and disparities. The research aims to identify which groups are most at risk through detailed statistical analysis, thereby informing targeted medical interventions and increasing awareness of the demographic variations in this chronic disease.
Methods: Data from the Nationwide Admission Database (HCUP) for 2019-2023 on 1,748,576 adult hospital admissions with a primary diagnosis of Eosinophilic esophagitis was analyzed. The study began with an inspection of the dataset's structure, emphasizing race, gender, and eosinophilic esophagitis indicators. Incidence rates were summarized by demographics, followed by chi-square tests to identify significant incidence variations among different racial and gender groups, using contingency tables for statistics and p-values. Logistic regression was then applied to further explore these associations, with race and gender as predictors, and eosinophilic esophagitis as the dependent outcome
Results: Between 2019 and 2023, 1,748,576 patients were admitted; 11051 Eosinophilic esophagitis patients were studied after propensity score matching. Logistic regression analysis highlights significant racial and gender disparities in eosinophilic esophagitis incidence. White individuals have the highest likelihood (coefficient: 2.2411, p< 0.0001), with Blacks also at increased risk (coefficient: 1.0911, p< 0.0001). Conversely, Other Races have a reduced likelihood (coefficient: -1.0702, p< 0.0001). No significant odds difference is seen in Hispanics (coefficient: -0.0102, p=0.9742). Males are less likely to develop the condition than females (coefficient: -0.1760, p< 0.0001), emphasizing race and gender's role in the disease's prevalence.
Discussion: The study highlights significant racial and gender disparities in eosinophilic esophagitis (EoE) incidence, emphasizing the need for tailored healthcare strategies. Increased prevalence among White and Black populations suggests potential genetic or environmental influences, while the higher incidence in females may indicate hormonal or immune variations. These findings support the development of customized medical approaches that consider these demographic factors to improve treatment outcomes and efficacy in EoE managemen
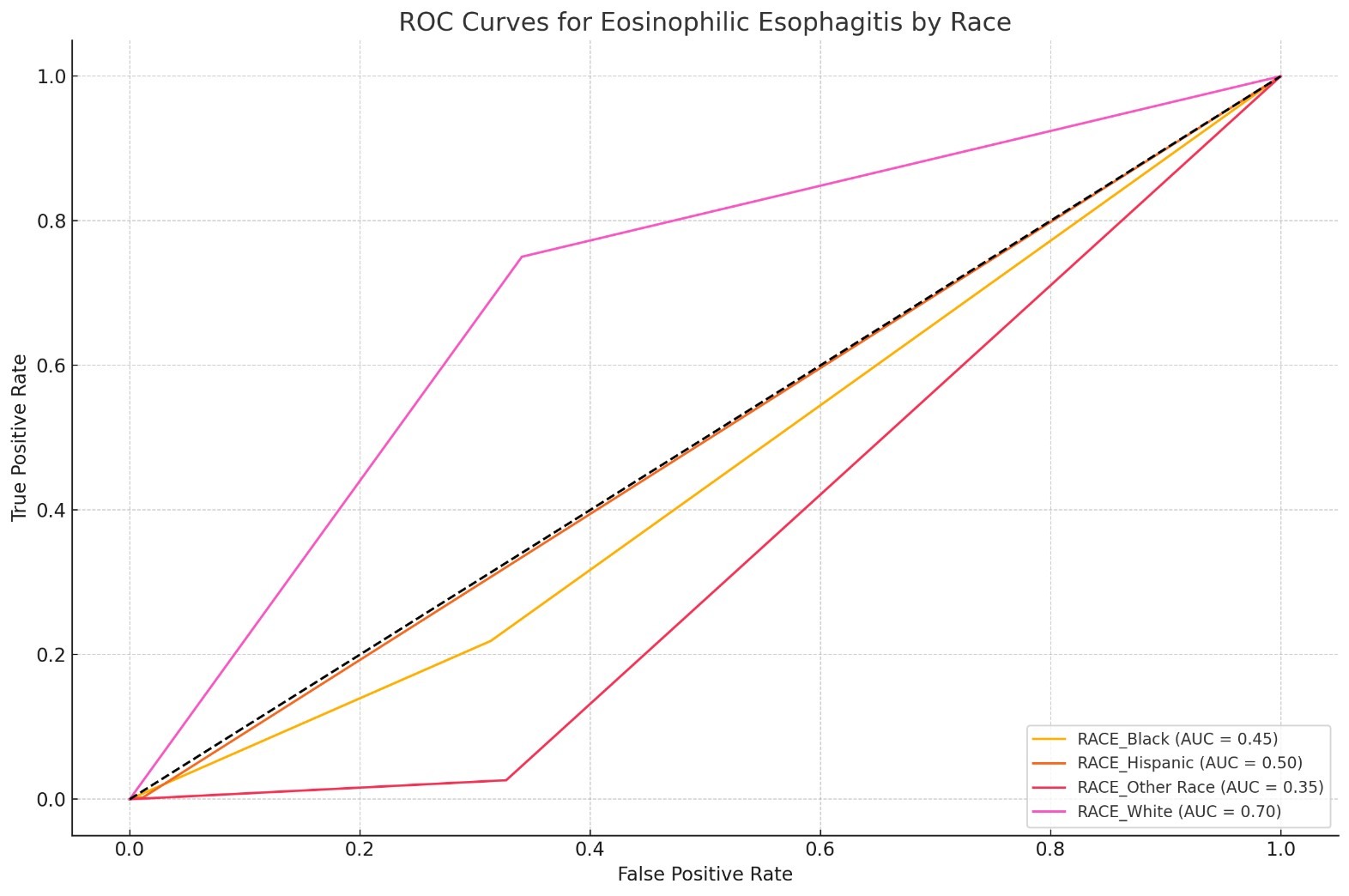
Figure: Eosinophilic esophagitis outcome among different races
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Raj Mohan Ram Mohan indicated no relevant financial relationships.
Sai Reshma Magam indicated no relevant financial relationships.
Sai Greeshma Magam indicated no relevant financial relationships.
Melvin Joy indicated no relevant financial relationships.
Dilman Natt indicated no relevant financial relationships.
Leeza Pannikodu indicated no relevant financial relationships.
Winghang Lau indicated no relevant financial relationships.
Abhishek Tadikonda indicated no relevant financial relationships.
Jiten Desai indicated no relevant financial relationships.
Krishnaiyer Subramani indicated no relevant financial relationships.
Paul Mustacchia indicated no relevant financial relationships.
Raj Mohan Ram Mohan, MD, Sai Reshma Magam, MD, Sai Greeshma Magam, MD, Melvin Joy, MD, Dilman Natt, MD, Leeza Pannikodu, MD, Winghang Lau, MD, Abhishek Tadikonda, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Paul Mustacchia, MD, MBA. P0487 - Exploring Demographic Variations in Eosinophilic Esophagitis: A Nationwide Study of Hospital Admissions From 2019-2023, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
