Sunday Poster Session
Category: Esophagus
P0505 - Defining the Natural History of Ineffective Esophageal Motility and Change in Diagnosis with Updated Chicago Classification Criteria
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ilora Naik, MD
Cedars-Sinai Medical Center
Los Angeles, CA
Presenting Author(s)
Ilora Naik, MD1, Bianca W. Chang, MD1, Jane Lim, MD1, Yin Chan, MD1, Mark Pimentel, MD2, Karthik Ravi, MD3, Amrit K.. Kamboj, MD1, Ali Rezaie, MD2
1Cedars-Sinai Medical Center, Los Angeles, CA; 2Cedars-Sinai Medical Center, West Hollywood, CA; 3Mayo Clinic, Rochester, MN
Introduction: Ineffective esophageal motility (IEM) is the most common abnormality seen on high-resolution esophageal manometries (HRMs). The diagnostic criteria for IEM based on Chicago classification (CC) have become more stringent over time. The aim of this study was to examine changes in IEM diagnosis over time to better define its natural history.
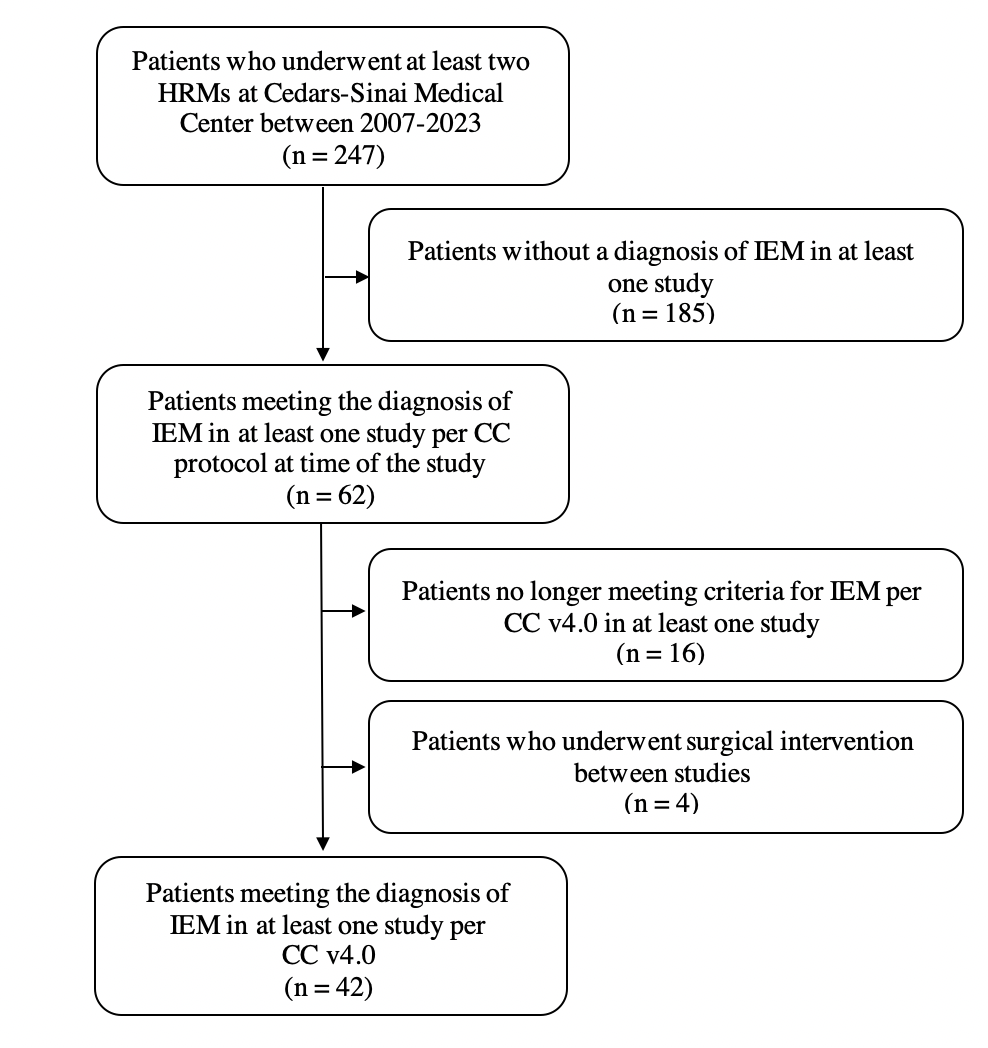
Methods: In this retrospective study, patients were included if they underwent at least two HRMs performed at a single institution between 2007-2023 with at least one study demonstrating IEM based on the CC diagnostic criteria at the time of the study. Patients that underwent surgical intervention of the esophagus between HRMs were excluded. All HRMs were performed using the Medtronics system and were interpreted by a gastroenterologist with expertise in esophageal motility disorders using the latest CC protocol at the time of the study. For patients meeting inclusion criteria, all HRMs were re-analyzed using CCv4.0 to determine how many patients retained IEM diagnosis with the updated criteria. In those that met IEM criteria per CCv4.0 on at least one study, alternate diagnoses were captured on the non-IEM HRM study using CCv4.0.
Results: The study cohort consisted of 62 patients who underwent at least two HRMs at a single institution and met criteria for IEM on at least one study based on the CC diagnostic criteria at the time of the study (Figure 1). Of these, 22 (35%) patients no longer met diagnostic criteria for IEM on at least one study based on CCv4.0; 6 of these 22 patients had another HRM that met criteria for IEM per CCv4.0. Table 1 outlines the patients that met IEM criteria for CCv4.0 on at least one study (n=42) and the alternate diagnoses before/after IEM diagnosis. Eighteen (43%) patients had IEM on both HRMs, 6 (14%) patients had IEM on the first HRM and normal esophageal motility on the second HRM, and 18 (43%) patients had normal esophageal motility on the first HRM and IEM on the second HRM. The median time between studies was 3.5 years representing 147 person-years. No patients with IEM progressed to achalasia, esophagogastric junction outflow obstruction, or absent contractility.
Discussion: One-third of patients with IEM based on earlier CC criteria were re-classified as having normal esophageal motility per CCv4.0. Patients with IEM appear to have a non-progressive disease course either retaining IEM diagnosis or having normal esophageal motility on repeat HRM without developing a major motility disorder.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ilora Naik, MD1, Bianca W. Chang, MD1, Jane Lim, MD1, Yin Chan, MD1, Mark Pimentel, MD2, Karthik Ravi, MD3, Amrit K.. Kamboj, MD1, Ali Rezaie, MD2. P0505 - Defining the Natural History of Ineffective Esophageal Motility and Change in Diagnosis with Updated Chicago Classification Criteria, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cedars-Sinai Medical Center, Los Angeles, CA; 2Cedars-Sinai Medical Center, West Hollywood, CA; 3Mayo Clinic, Rochester, MN
Introduction: Ineffective esophageal motility (IEM) is the most common abnormality seen on high-resolution esophageal manometries (HRMs). The diagnostic criteria for IEM based on Chicago classification (CC) have become more stringent over time. The aim of this study was to examine changes in IEM diagnosis over time to better define its natural history.
Methods: In this retrospective study, patients were included if they underwent at least two HRMs performed at a single institution between 2007-2023 with at least one study demonstrating IEM based on the CC diagnostic criteria at the time of the study. Patients that underwent surgical intervention of the esophagus between HRMs were excluded. All HRMs were performed using the Medtronics system and were interpreted by a gastroenterologist with expertise in esophageal motility disorders using the latest CC protocol at the time of the study. For patients meeting inclusion criteria, all HRMs were re-analyzed using CCv4.0 to determine how many patients retained IEM diagnosis with the updated criteria. In those that met IEM criteria per CCv4.0 on at least one study, alternate diagnoses were captured on the non-IEM HRM study using CCv4.0.
Results: The study cohort consisted of 62 patients who underwent at least two HRMs at a single institution and met criteria for IEM on at least one study based on the CC diagnostic criteria at the time of the study (Figure 1). Of these, 22 (35%) patients no longer met diagnostic criteria for IEM on at least one study based on CCv4.0; 6 of these 22 patients had another HRM that met criteria for IEM per CCv4.0. Table 1 outlines the patients that met IEM criteria for CCv4.0 on at least one study (n=42) and the alternate diagnoses before/after IEM diagnosis. Eighteen (43%) patients had IEM on both HRMs, 6 (14%) patients had IEM on the first HRM and normal esophageal motility on the second HRM, and 18 (43%) patients had normal esophageal motility on the first HRM and IEM on the second HRM. The median time between studies was 3.5 years representing 147 person-years. No patients with IEM progressed to achalasia, esophagogastric junction outflow obstruction, or absent contractility.
Discussion: One-third of patients with IEM based on earlier CC criteria were re-classified as having normal esophageal motility per CCv4.0. Patients with IEM appear to have a non-progressive disease course either retaining IEM diagnosis or having normal esophageal motility on repeat HRM without developing a major motility disorder.
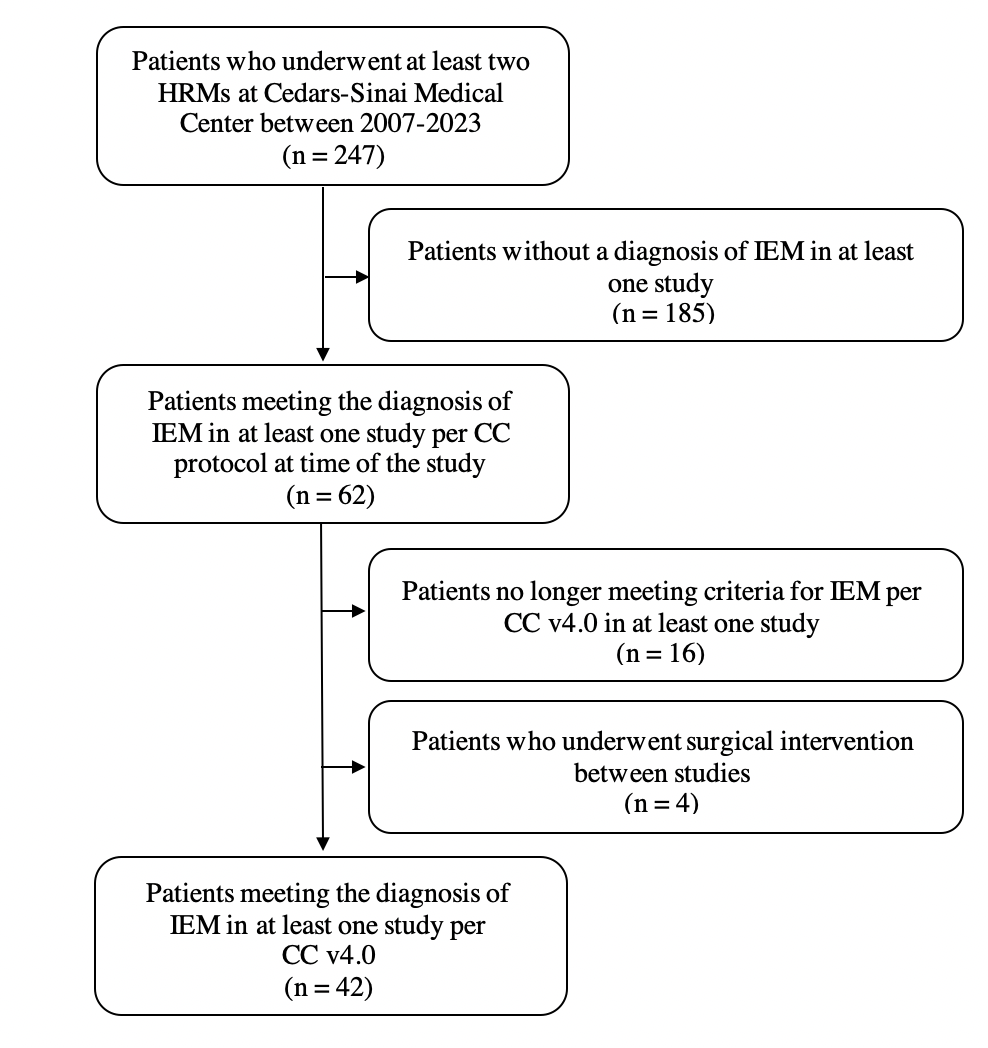
Figure: Study flow diagram
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ilora Naik indicated no relevant financial relationships.
Bianca Chang indicated no relevant financial relationships.
Jane Lim indicated no relevant financial relationships.
Yin Chan indicated no relevant financial relationships.
Mark Pimentel: Cylinder Health – Consultant, Stock Options. Dieta Health – Consultant, Stock Options. Ferring – Consultant. Gemelli Biotech – Advisory Committee/Board Member, Intellectual Property/Patents, Stock-privately held company. GoodLFE – Consultant, Stock-privately held company. Salvo Health – Consultant, Stock Options.
Karthik Ravi indicated no relevant financial relationships.
Amrit Kamboj: Castle Biosciences – Consultant.
Ali Rezaie: Ardelyx – Consultant. Bausch Health – Consultant, Speakers Bureau. Gemelli Biotech – Stock-privately held company. GoodLFE – Stock-privately held company.
Ilora Naik, MD1, Bianca W. Chang, MD1, Jane Lim, MD1, Yin Chan, MD1, Mark Pimentel, MD2, Karthik Ravi, MD3, Amrit K.. Kamboj, MD1, Ali Rezaie, MD2. P0505 - Defining the Natural History of Ineffective Esophageal Motility and Change in Diagnosis with Updated Chicago Classification Criteria, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

