Sunday Poster Session
Category: Esophagus
P0510 - Cholecystectomy Is Associated With Reduced Risk of Esophageal Cancer: A Multi-Center Research Network Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Prabhat Kumar, MD
Cleveland Clinic Foundation
Richmond, VA
Presenting Author(s)
Prabhat Kumar, MD1, Thabet Qapaja, MD1, Archana Kharel, MD1, Islam B Mohamed, MD1, Mohamad-Noor Abu-Hammour, MD2, Mohamed Nadeem, MD1, Madhusudhan R. Sanaka, MD1, Prashanthi N. Thota, MD1
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Fairview, Cleveland, OH
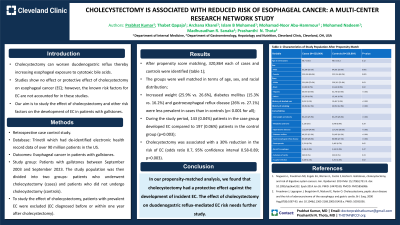
Introduction: Cholecystectomy can worsen duodenogastric reflux thereby increasing esophageal exposure to cytotoxic bile acids. Studies show no effect or protective effect of cholecystectomy on esophageal cancer (EC); however, the known risk factors for EC are not accounted for in these studies. Therefore, our aim was to study the effect of cholecystectomy and other risk factors on the development of EC in patients with gallstones.
Methods: The TriNetX platform, a federated health research network that aggregates de-identified electronic health record data of over 90 million patients across the United States, was queried for patients with gallstones between September 2003 and September 2023. The study population was then divided into two groups: patients who underwent cholecystectomy (cases) and patients who did not undergo cholecystectomy (controls). To study the effect of cholecystectomy, patients with prevalent EC were excluded (EC diagnosed before or within one year after cholecystectomy).
Results: After propensity score matching, 320,864 each of cases and controls were identified (table). The groups were well matched in terms of age, sex, and racial distribution. Increased weight (25.9% vs. 26.6%), diabetes mellitus (15.3% vs. 16.2%) and gastroesophageal reflux disease (26% vs. 27.1%) were less prevalent in cases than in controls (p< 0.001 for all). During the study period, 143 (0.04%) patients in the case group developed EC compared to 197 (0.06%) patients in the control group (p=0.003). Cholecystectomy was associated with a 30% reduction in the risk of EC (odds ratio 0.7, 95% confidence interval 0.58-0.89; p=0.003).
Discussion: In our propensity-matched analysis, we found that cholecystectomy had a protective effect against the development of incident EC. The effect of cholecystectomy on duodenogastric reflux mediated EC risk needs further study.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Prabhat Kumar, MD1, Thabet Qapaja, MD1, Archana Kharel, MD1, Islam B Mohamed, MD1, Mohamad-Noor Abu-Hammour, MD2, Mohamed Nadeem, MD1, Madhusudhan R. Sanaka, MD1, Prashanthi N. Thota, MD1. P0510 - Cholecystectomy Is Associated With Reduced Risk of Esophageal Cancer: A Multi-Center Research Network Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Fairview, Cleveland, OH
Introduction: Cholecystectomy can worsen duodenogastric reflux thereby increasing esophageal exposure to cytotoxic bile acids. Studies show no effect or protective effect of cholecystectomy on esophageal cancer (EC); however, the known risk factors for EC are not accounted for in these studies. Therefore, our aim was to study the effect of cholecystectomy and other risk factors on the development of EC in patients with gallstones.
Methods: The TriNetX platform, a federated health research network that aggregates de-identified electronic health record data of over 90 million patients across the United States, was queried for patients with gallstones between September 2003 and September 2023. The study population was then divided into two groups: patients who underwent cholecystectomy (cases) and patients who did not undergo cholecystectomy (controls). To study the effect of cholecystectomy, patients with prevalent EC were excluded (EC diagnosed before or within one year after cholecystectomy).
Results: After propensity score matching, 320,864 each of cases and controls were identified (table). The groups were well matched in terms of age, sex, and racial distribution. Increased weight (25.9% vs. 26.6%), diabetes mellitus (15.3% vs. 16.2%) and gastroesophageal reflux disease (26% vs. 27.1%) were less prevalent in cases than in controls (p< 0.001 for all). During the study period, 143 (0.04%) patients in the case group developed EC compared to 197 (0.06%) patients in the control group (p=0.003). Cholecystectomy was associated with a 30% reduction in the risk of EC (odds ratio 0.7, 95% confidence interval 0.58-0.89; p=0.003).
Discussion: In our propensity-matched analysis, we found that cholecystectomy had a protective effect against the development of incident EC. The effect of cholecystectomy on duodenogastric reflux mediated EC risk needs further study.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Prabhat Kumar indicated no relevant financial relationships.
Thabet Qapaja indicated no relevant financial relationships.
Archana Kharel indicated no relevant financial relationships.
Islam B Mohamed indicated no relevant financial relationships.
Mohamad-Noor Abu-Hammour indicated no relevant financial relationships.
Mohamed Nadeem indicated no relevant financial relationships.
Madhusudhan R. Sanaka indicated no relevant financial relationships.
Prashanthi Thota indicated no relevant financial relationships.
Prabhat Kumar, MD1, Thabet Qapaja, MD1, Archana Kharel, MD1, Islam B Mohamed, MD1, Mohamad-Noor Abu-Hammour, MD2, Mohamed Nadeem, MD1, Madhusudhan R. Sanaka, MD1, Prashanthi N. Thota, MD1. P0510 - Cholecystectomy Is Associated With Reduced Risk of Esophageal Cancer: A Multi-Center Research Network Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
