Sunday Poster Session
Category: Esophagus
P0537 - Acute Pseudoachalasia After Catheter Ablation for Atrial Fibrillation
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Brandon T. Wiggins, DO, MPH
Ascension Genesys Hospital
Grand Blanc, MI
Presenting Author(s)
Brandon T. Wiggins, DO, MPH1, Mai Phuong Truong, MD2, Se Yeon Kim, DO3, Jake Burch, DO4, Justin Miller, DO5
1Ascension Genesys Hospital, Grand Blanc, MI; 2Ascension Genesys, Holly, MI; 3Ascension Genesys, Grand Blanc, MI; 4Ascension Genesys, Swartz Creek, MI; 5Ascension Genesys Hospital, Clarkston, MI
Introduction: Pseudoachalasia (PA), a rare disorder of the esophagus, is characterized by the persistent contraction of the lower esophageal sphincter. Patients with PA may exhibit dysphagia, regurgitation, chest pain, and weight loss. Despite the majority of PA cases being idiopathic, etiologies can also be genetic, autoimmune or iatrogenic. Although pathophysiology of PA is still unclear, the degeneration of the vagus nerve and its influence on Auerbach's and Meissner's plexuses are key in its development. Studies have rarely reported vagus nerve injury as a potential complication of catheter ablation (CA) for atrial fibrillation (AF).
Case Description/Methods: 72 year old male with AF presented for isolated fevers and chills for one week. He had CA for atrial fibrillation 2 weeks prior without complication. He had an extensive workup for fever that was unremarkable except for pulmonary nodules on imaging and ruled out atrial esophageal fistula. He was empirically treated with antibiotics. Gastroenterology was eventually consulted after he developed acute dysphagia to solids and liquids, as well as regurgitation.
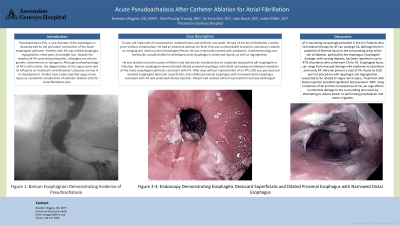
He was started on proton pump inhibitors and had diet de-escalated due to suspected doxycycline pill esophagitis or infection. Barium esophagram demonstrated dilated proximal esophagus with distal narrowing and delayed relaxation of the lower esophageal sphincter consistent with PA. After days without improvement of on PPI, EGD was pursued and revealed esophagitis desiccant superficialis, and a dilated proximal esophagus with narrowed distal esophagus consistent with PA and underwent Botox injection. Patient had marked clinical improvement and was discharged.
Discussion: AF is becoming increasingly prevalent in the US. Patients who fail medical therapy for AF can undergo CA, although there is potential of thermal injury to the surrounding areas of the site of ablation, particularly the esophagus. Esophageal damage, with varying degrees, has been reported in up to 47% of patients who underwent CA for AF. Esophageal injury can range from mucosal damage with erythema to ulceration and rarely PA. Here we present a case of PA, found on EGD, post CA procedure with dysphagia and regurgitation, suspected to be related to vagus nerve injury. Treatment with Botox injection provided significant improvement. With rising incidences of AF and the increased use of CA, we urge efforts to minimize damage to the surrounding structures by attempting to reduce power or performing prophylactic cool water irrigation.

Disclosures:
Brandon T. Wiggins, DO, MPH1, Mai Phuong Truong, MD2, Se Yeon Kim, DO3, Jake Burch, DO4, Justin Miller, DO5. P0537 - Acute Pseudoachalasia After Catheter Ablation for Atrial Fibrillation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Ascension Genesys Hospital, Grand Blanc, MI; 2Ascension Genesys, Holly, MI; 3Ascension Genesys, Grand Blanc, MI; 4Ascension Genesys, Swartz Creek, MI; 5Ascension Genesys Hospital, Clarkston, MI
Introduction: Pseudoachalasia (PA), a rare disorder of the esophagus, is characterized by the persistent contraction of the lower esophageal sphincter. Patients with PA may exhibit dysphagia, regurgitation, chest pain, and weight loss. Despite the majority of PA cases being idiopathic, etiologies can also be genetic, autoimmune or iatrogenic. Although pathophysiology of PA is still unclear, the degeneration of the vagus nerve and its influence on Auerbach's and Meissner's plexuses are key in its development. Studies have rarely reported vagus nerve injury as a potential complication of catheter ablation (CA) for atrial fibrillation (AF).
Case Description/Methods: 72 year old male with AF presented for isolated fevers and chills for one week. He had CA for atrial fibrillation 2 weeks prior without complication. He had an extensive workup for fever that was unremarkable except for pulmonary nodules on imaging and ruled out atrial esophageal fistula. He was empirically treated with antibiotics. Gastroenterology was eventually consulted after he developed acute dysphagia to solids and liquids, as well as regurgitation.
He was started on proton pump inhibitors and had diet de-escalated due to suspected doxycycline pill esophagitis or infection. Barium esophagram demonstrated dilated proximal esophagus with distal narrowing and delayed relaxation of the lower esophageal sphincter consistent with PA. After days without improvement of on PPI, EGD was pursued and revealed esophagitis desiccant superficialis, and a dilated proximal esophagus with narrowed distal esophagus consistent with PA and underwent Botox injection. Patient had marked clinical improvement and was discharged.
Discussion: AF is becoming increasingly prevalent in the US. Patients who fail medical therapy for AF can undergo CA, although there is potential of thermal injury to the surrounding areas of the site of ablation, particularly the esophagus. Esophageal damage, with varying degrees, has been reported in up to 47% of patients who underwent CA for AF. Esophageal injury can range from mucosal damage with erythema to ulceration and rarely PA. Here we present a case of PA, found on EGD, post CA procedure with dysphagia and regurgitation, suspected to be related to vagus nerve injury. Treatment with Botox injection provided significant improvement. With rising incidences of AF and the increased use of CA, we urge efforts to minimize damage to the surrounding structures by attempting to reduce power or performing prophylactic cool water irrigation.

Figure: Barium Esophagram Demonstrating Evidence of Pseudoachalasia
Disclosures:
Brandon Wiggins indicated no relevant financial relationships.
Mai Phuong Truong indicated no relevant financial relationships.
Se Yeon Kim indicated no relevant financial relationships.
Jake Burch indicated no relevant financial relationships.
Justin Miller indicated no relevant financial relationships.
Brandon T. Wiggins, DO, MPH1, Mai Phuong Truong, MD2, Se Yeon Kim, DO3, Jake Burch, DO4, Justin Miller, DO5. P0537 - Acute Pseudoachalasia After Catheter Ablation for Atrial Fibrillation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
