Sunday Poster Session
Category: Esophagus
P0539 - Management of Gastrointestinal Bleeding Due to Esophageal Varices Utilizing Metallic Esophageal Stent
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- LD
Layla Darwiche, BA
Henry Ford Health
Detroit, MI
Presenting Author(s)
Layla Darwiche, BA, Taha Ashraf, MD, Syed-Mohammed Jafri, MD
Henry Ford Health, Detroit, MI
Introduction: We present an unusual case of esophageal varices and refractory gastrointestinal bleeding managed with placement of esophageal stents.
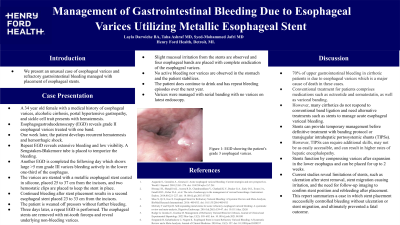
Case Description/Methods: A 34 year old female with a medical history of esophageal varices, alcoholic cirrhosis, portal hypertensive gastropathy, and sickle cell trait presents with hematemesis. Esophagogastroduodenoscopy (EGD) reveals grade II esophageal varices treated with one band. One week later, the patient develops recurrent hematemesis and hemorrhagic shock. Repeat EGD reveals extensive bleeding and low visibility. A Sengstaken-Blakemore tube is placed to temporize the bleeding. Another EGD is completed the following day which shows large >5 mm grade III varices bleeding actively in the lower one-third of the esophagus. The varices are stented with a metallic esophageal stent coated in silicone, placed 25 to 37 cm from the incisors, and two hemostatic clips are placed to keep the stent in place. Continued bleeding after stent placement results in a second esophageal stent placed 23 to 33 cm from the incisors. The patient is weaned off pressors without further bleeding.
Three days later, a repeat EGD is performed. The esophageal stents are removed with rat-tooth forceps and reveal underlying non-bleeding varices. Slight mucosal irritation from the stents are observed and four esophageal bands are placed with complete eradication of the esophageal varices. No active bleeding nor varices are observed in the stomach and the patient stabilizes. The patient does continue to drink and has repeat bleeding episodes over the next year. Varices were managed with serial banding with no varices on latest endoscopy.
Discussion: Many cirrhotics do not respond to conventional band ligation and need alternative treatments such as stents to manage acute esophageal variceal bleeding. Stents can provide temporary management before definitive treatment with banding protocol or transjugular intrahepatic portosystemic shunts (TIPSs). Stents function by compressing varices after expansion in the lower esophagus. Current studies reveal limitations of stents, such as ulceration after stent removal, stent migration causing irritation, and the need for follow-up imaging to confirm stent position and rebleeding. This report summarizes a case in which stent placement successfully controlled bleeding without ulceration or stent migration, and ultimately prevented a fatal outcome.
Disclosures:
Layla Darwiche, BA, Taha Ashraf, MD, Syed-Mohammed Jafri, MD. P0539 - Management of Gastrointestinal Bleeding Due to Esophageal Varices Utilizing Metallic Esophageal Stent, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Henry Ford Health, Detroit, MI
Introduction: We present an unusual case of esophageal varices and refractory gastrointestinal bleeding managed with placement of esophageal stents.
Case Description/Methods: A 34 year old female with a medical history of esophageal varices, alcoholic cirrhosis, portal hypertensive gastropathy, and sickle cell trait presents with hematemesis. Esophagogastroduodenoscopy (EGD) reveals grade II esophageal varices treated with one band. One week later, the patient develops recurrent hematemesis and hemorrhagic shock. Repeat EGD reveals extensive bleeding and low visibility. A Sengstaken-Blakemore tube is placed to temporize the bleeding. Another EGD is completed the following day which shows large >5 mm grade III varices bleeding actively in the lower one-third of the esophagus. The varices are stented with a metallic esophageal stent coated in silicone, placed 25 to 37 cm from the incisors, and two hemostatic clips are placed to keep the stent in place. Continued bleeding after stent placement results in a second esophageal stent placed 23 to 33 cm from the incisors. The patient is weaned off pressors without further bleeding.
Three days later, a repeat EGD is performed. The esophageal stents are removed with rat-tooth forceps and reveal underlying non-bleeding varices. Slight mucosal irritation from the stents are observed and four esophageal bands are placed with complete eradication of the esophageal varices. No active bleeding nor varices are observed in the stomach and the patient stabilizes. The patient does continue to drink and has repeat bleeding episodes over the next year. Varices were managed with serial banding with no varices on latest endoscopy.
Discussion: Many cirrhotics do not respond to conventional band ligation and need alternative treatments such as stents to manage acute esophageal variceal bleeding. Stents can provide temporary management before definitive treatment with banding protocol or transjugular intrahepatic portosystemic shunts (TIPSs). Stents function by compressing varices after expansion in the lower esophagus. Current studies reveal limitations of stents, such as ulceration after stent removal, stent migration causing irritation, and the need for follow-up imaging to confirm stent position and rebleeding. This report summarizes a case in which stent placement successfully controlled bleeding without ulceration or stent migration, and ultimately prevented a fatal outcome.
Disclosures:
Layla Darwiche indicated no relevant financial relationships.
Taha Ashraf indicated no relevant financial relationships.
Syed-Mohammed Jafri: Gilead, Takeda, Abbvie, Intercept, VectivBio – Advisor or Review Panel Member, Speakers Bureau.
Layla Darwiche, BA, Taha Ashraf, MD, Syed-Mohammed Jafri, MD. P0539 - Management of Gastrointestinal Bleeding Due to Esophageal Varices Utilizing Metallic Esophageal Stent, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
