Sunday Poster Session
Category: Esophagus
P0597 - A Rare Case of Gastrobronchial Fistula Following Minimally Invasive Esophagectomy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Urmimala Chaudhuri, DO
Wright State University
Centerville, OH
Presenting Author(s)
Urmimala Chaudhuri, DO1, Bahar Cheema, MD2, Mustafa Musleh, MD3
1Wright State University, Centerville, OH; 2Kettering Health, Centerville, OH; 3Digestive Specialists, Dayton, OH
Introduction: A gastrobronchial fistula (GBF) is a rare condition that can result as a complication after a surgical procedure. We present a rare case of a patient who was diagnosed with a GBF complication after minimally invasive distal esophagectomy. We discuss the presentation of GBF and approach to conservative management.
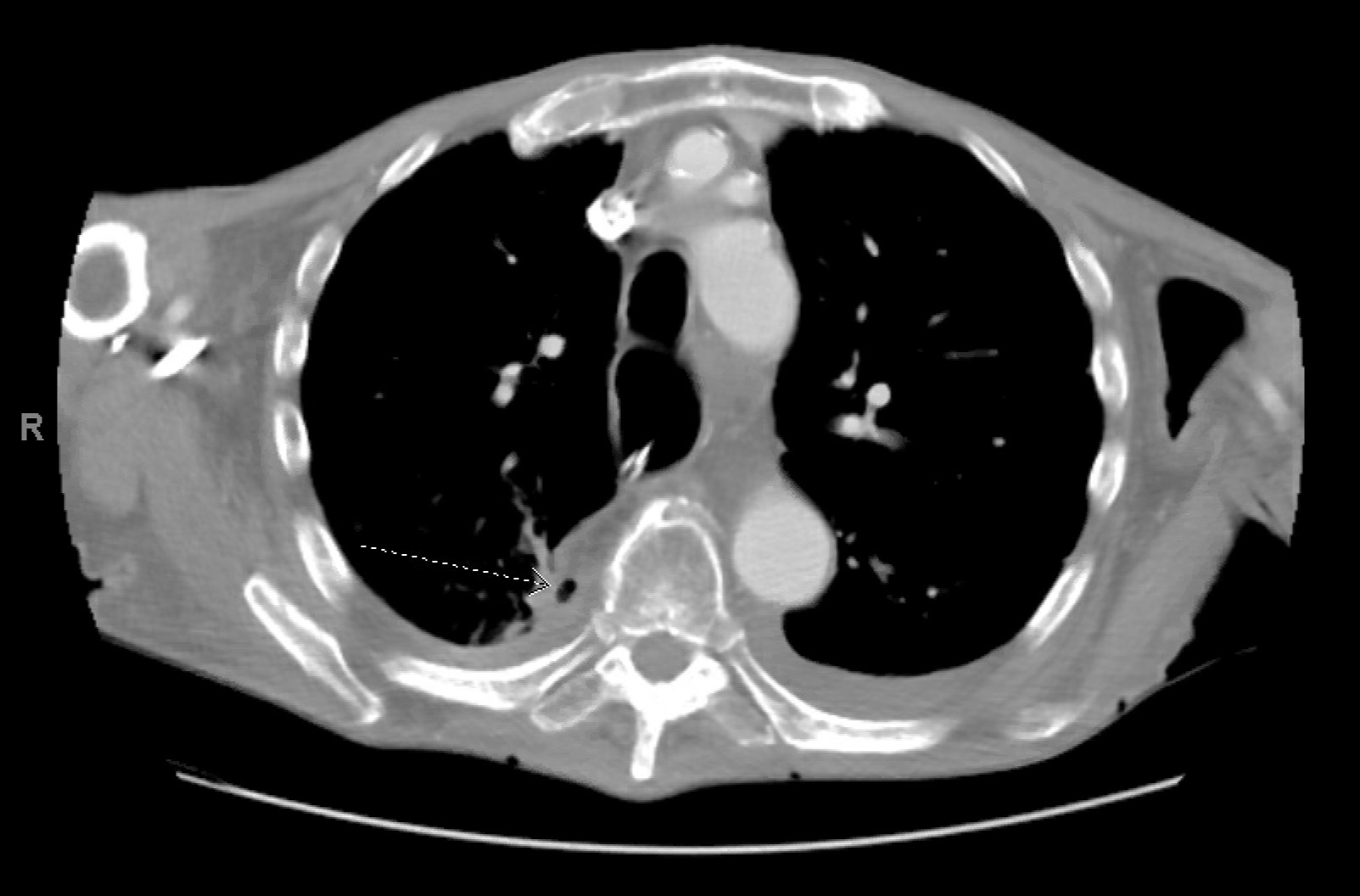
Case Description/Methods: 78-year-old male was diagnosed with esophageal adenocarcinoma for which he underwent minimally invasive esophagectomy with intrathoracic anastomosis. On postop day 14, the patient returned to the ED for concerns of sepsis. The patient was found to have evidence of an anastomotic leak on imaging. He underwent an EGD which revealed a segment of necrotic appearing gastric mucosa below gastroesophageal anastomosis. An esophageal stent was placed to treat a large leak found in the gastric conduit distal to the anastomosis. The stent was removed three months later as chest imaging did not reveal an anastomotic leak around the stent. 18 months later, the patient was referred back to gastroenterology after an esophagogram revealed concerns for food retention proximal to the anastomosis. He underwent an EGD which revealed chronic gastric ulceration along with two definitive areas of perforation. An esophagogram revealed slow extravasation from the stomach filling bronchial structures in the right upper and middle lobe of the lung consistent with GBF. The patient opted for a conservative approach by electing stent placement from the esophagus to the distal stomach. Fistula closure was attempted with a metal stent that was deployed in the esophagus and anchored in the esophagus by endoscopic tack to prevent stent migration. Post-procedure esophagogram did not reveal gastric contents in the right upper and middle lobes. The patient was discharged in stable condition with the recommendation of strict NPO and tube feeds via jejunostomy.
Discussion: This case highlights a rare complication of esophagectomy which is GBF. Treatment strategies depend on the location and size of the fistula along with the patient’s functional status. Non-surgical methods include esophageal stents such as self-expandable stents, over-the-scope clips, or silicon stents. Definitive treatment for GBF is surgical repair. We highlight a conservative approach to treating GBF by utilizing an endoscopic technique with a self-expanding fully covered metal. The risk of stent migration is mitigated by anchoring the stent with endoscopic tack and using a fully covered stent with anti-migration struts.
Disclosures:
Urmimala Chaudhuri, DO1, Bahar Cheema, MD2, Mustafa Musleh, MD3. P0597 - A Rare Case of Gastrobronchial Fistula Following Minimally Invasive Esophagectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Wright State University, Centerville, OH; 2Kettering Health, Centerville, OH; 3Digestive Specialists, Dayton, OH
Introduction: A gastrobronchial fistula (GBF) is a rare condition that can result as a complication after a surgical procedure. We present a rare case of a patient who was diagnosed with a GBF complication after minimally invasive distal esophagectomy. We discuss the presentation of GBF and approach to conservative management.
Case Description/Methods: 78-year-old male was diagnosed with esophageal adenocarcinoma for which he underwent minimally invasive esophagectomy with intrathoracic anastomosis. On postop day 14, the patient returned to the ED for concerns of sepsis. The patient was found to have evidence of an anastomotic leak on imaging. He underwent an EGD which revealed a segment of necrotic appearing gastric mucosa below gastroesophageal anastomosis. An esophageal stent was placed to treat a large leak found in the gastric conduit distal to the anastomosis. The stent was removed three months later as chest imaging did not reveal an anastomotic leak around the stent. 18 months later, the patient was referred back to gastroenterology after an esophagogram revealed concerns for food retention proximal to the anastomosis. He underwent an EGD which revealed chronic gastric ulceration along with two definitive areas of perforation. An esophagogram revealed slow extravasation from the stomach filling bronchial structures in the right upper and middle lobe of the lung consistent with GBF. The patient opted for a conservative approach by electing stent placement from the esophagus to the distal stomach. Fistula closure was attempted with a metal stent that was deployed in the esophagus and anchored in the esophagus by endoscopic tack to prevent stent migration. Post-procedure esophagogram did not reveal gastric contents in the right upper and middle lobes. The patient was discharged in stable condition with the recommendation of strict NPO and tube feeds via jejunostomy.
Discussion: This case highlights a rare complication of esophagectomy which is GBF. Treatment strategies depend on the location and size of the fistula along with the patient’s functional status. Non-surgical methods include esophageal stents such as self-expandable stents, over-the-scope clips, or silicon stents. Definitive treatment for GBF is surgical repair. We highlight a conservative approach to treating GBF by utilizing an endoscopic technique with a self-expanding fully covered metal. The risk of stent migration is mitigated by anchoring the stent with endoscopic tack and using a fully covered stent with anti-migration struts.
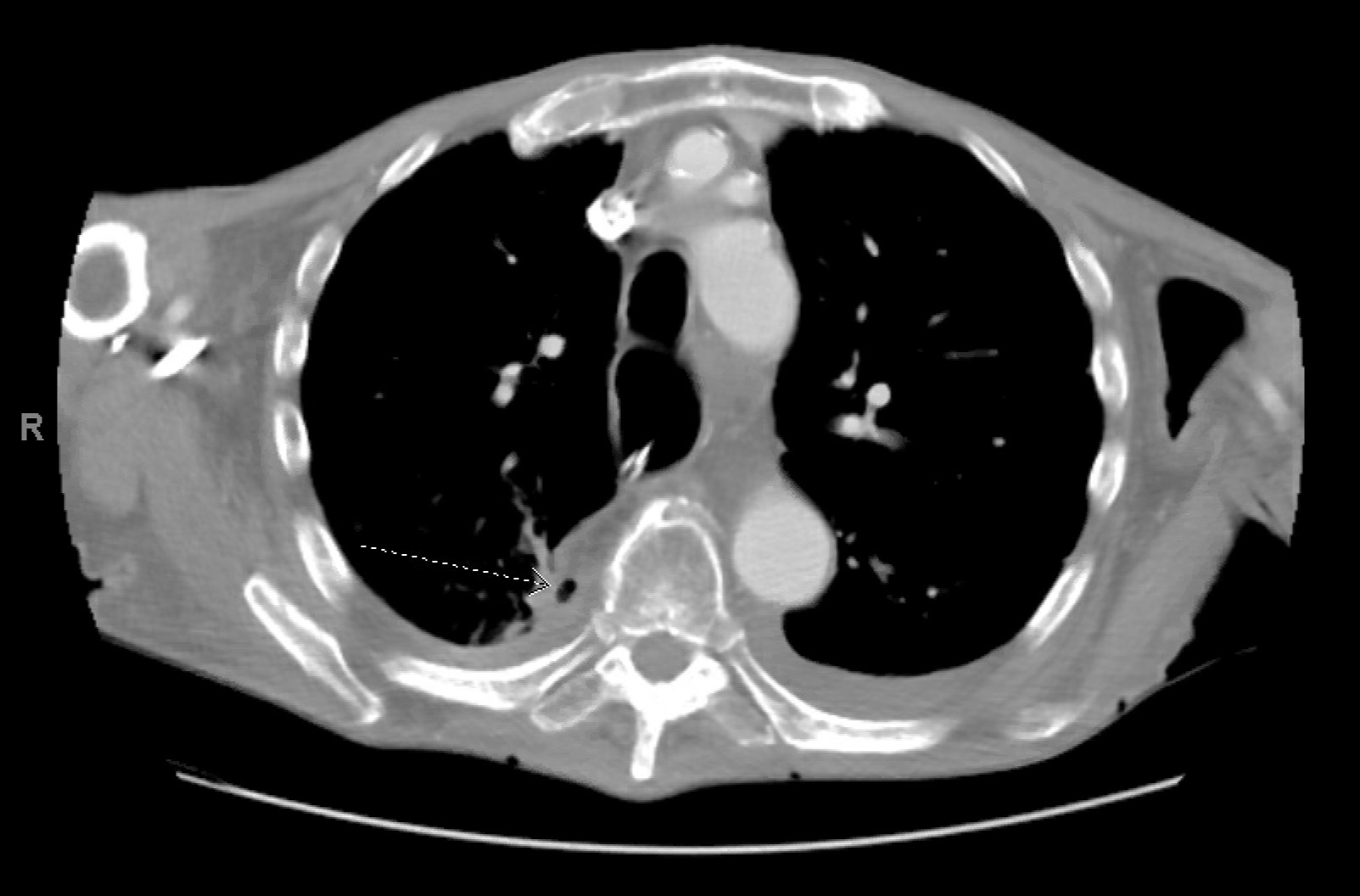
Figure: CT chest with contrast illustrating gastrobronchial fistula
Disclosures:
Urmimala Chaudhuri indicated no relevant financial relationships.
Bahar Cheema indicated no relevant financial relationships.
Mustafa Musleh indicated no relevant financial relationships.
Urmimala Chaudhuri, DO1, Bahar Cheema, MD2, Mustafa Musleh, MD3. P0597 - A Rare Case of Gastrobronchial Fistula Following Minimally Invasive Esophagectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
