Sunday Poster Session
Category: Esophagus
P0603 - Case Report: Esophagogastric Junction Outflow Obstruction Due to Infiltrative Amyloidosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Naomi Reddy-Patel, MD
St. Luke's University Hospital
Bethlehem, PA
Presenting Author(s)
Naomi Reddy-Patel, MD1, Ashton Ellison, MBBCh2, Pallavi Patil, MD3, Vani J.A.. Konda, MD2
1St. Luke's University Hospital, Bethlehem, PA; 2Baylor University Medical Center and Center for Esophageal Research, Baylor Scott & White Research Institute, Dallas, TX; 3Center for Esophageal Diseases, Baylor University Medical Center, Dallas, TX
Introduction: Esophagogastric junction outflow obstruction (EGJOO) is a manometric derived diagnosis and is a disorder of outflow obstruction in which the criteria for achalasia is not met. Although EGJOO is often considered an esophageal motility disorder, the etiologies include a heterogenous group of conditions, also including intrinsic diseases within the esophagus and extrinsic causes at the hiatus. We describe a case of EGJOO with an intrinsic infiltrative disease caused by amyloidosis
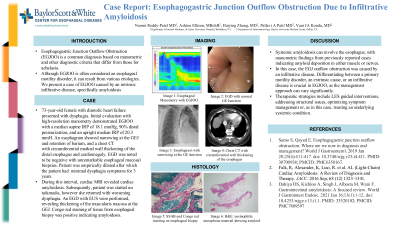
Case Description/Methods: A 73-year-old female with a history of atrial fibrillation and diastolic heart failure presented with dysphagia. She endorsed food and liquid dysphagia, post -prandial bloating, and regurgitation. Initial evaluation demonstrated an esophagogastroduodenoscopy (EGD) without stricture, an esophagram with narrowing at the GEJ and retention of barium, and a chest CT with circumferential marked wall thickening of the distal esophagus and cardiomegaly. A high resolution manometry demonstrated EGJOO with a median supine IRP of 18.1 mmHg, 90% distal pressurization, and an upright median IRP of 20.3 mmHg. Peristalsis ranged from intact in some swallows to failed in one swallow and hypercontractile in one. An EGD with FLIP demonstrated a non-obstructive endoscopic examination and reduced esophageal opening on panometry with a max diameter of 6.2 mm and distensibility-index of 0.7 mm2/mmHg at the 60 mL fill volume. Esophageal mucosal biopsies were unremarkable. A 20 mm dilation was performed after which the patient did well with minimal dysphagia symptoms for 3 years. During this interval, she developed shortness of breath and worsening cardiac issues. Ultimately, a cardiac MRI revealed cardiac amyloidosis, and she was treated with tafamidis. Subsequently, she returned with worsening dysphagia. An EGD with dilation and an endoscopic ultrasound were performed, revealing thickening of the muscularis mucosa at the GEJ. Congo red staining of tissue from esophageal biopsy was positive indicating amyloidosis
Discussion: Systemic amyloidosis may involve the esophagus. Manometric findings from previously published cases of amyloidosis involving the esophagus suggest amyloid deposition in both muscle or nerves. In this case, the cause of the EGJ outflow obstruction was due to an infiltrative disease. Differentiating between a primary motility disorder, an extrinsic cause, or an infiltrative disease is crucial in EGJOO, as the focus of management can differ substantially
Disclosures:
Naomi Reddy-Patel, MD1, Ashton Ellison, MBBCh2, Pallavi Patil, MD3, Vani J.A.. Konda, MD2. P0603 - Case Report: Esophagogastric Junction Outflow Obstruction Due to Infiltrative Amyloidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Luke's University Hospital, Bethlehem, PA; 2Baylor University Medical Center and Center for Esophageal Research, Baylor Scott & White Research Institute, Dallas, TX; 3Center for Esophageal Diseases, Baylor University Medical Center, Dallas, TX
Introduction: Esophagogastric junction outflow obstruction (EGJOO) is a manometric derived diagnosis and is a disorder of outflow obstruction in which the criteria for achalasia is not met. Although EGJOO is often considered an esophageal motility disorder, the etiologies include a heterogenous group of conditions, also including intrinsic diseases within the esophagus and extrinsic causes at the hiatus. We describe a case of EGJOO with an intrinsic infiltrative disease caused by amyloidosis
Case Description/Methods: A 73-year-old female with a history of atrial fibrillation and diastolic heart failure presented with dysphagia. She endorsed food and liquid dysphagia, post -prandial bloating, and regurgitation. Initial evaluation demonstrated an esophagogastroduodenoscopy (EGD) without stricture, an esophagram with narrowing at the GEJ and retention of barium, and a chest CT with circumferential marked wall thickening of the distal esophagus and cardiomegaly. A high resolution manometry demonstrated EGJOO with a median supine IRP of 18.1 mmHg, 90% distal pressurization, and an upright median IRP of 20.3 mmHg. Peristalsis ranged from intact in some swallows to failed in one swallow and hypercontractile in one. An EGD with FLIP demonstrated a non-obstructive endoscopic examination and reduced esophageal opening on panometry with a max diameter of 6.2 mm and distensibility-index of 0.7 mm2/mmHg at the 60 mL fill volume. Esophageal mucosal biopsies were unremarkable. A 20 mm dilation was performed after which the patient did well with minimal dysphagia symptoms for 3 years. During this interval, she developed shortness of breath and worsening cardiac issues. Ultimately, a cardiac MRI revealed cardiac amyloidosis, and she was treated with tafamidis. Subsequently, she returned with worsening dysphagia. An EGD with dilation and an endoscopic ultrasound were performed, revealing thickening of the muscularis mucosa at the GEJ. Congo red staining of tissue from esophageal biopsy was positive indicating amyloidosis
Discussion: Systemic amyloidosis may involve the esophagus. Manometric findings from previously published cases of amyloidosis involving the esophagus suggest amyloid deposition in both muscle or nerves. In this case, the cause of the EGJ outflow obstruction was due to an infiltrative disease. Differentiating between a primary motility disorder, an extrinsic cause, or an infiltrative disease is crucial in EGJOO, as the focus of management can differ substantially
Disclosures:
Naomi Reddy-Patel indicated no relevant financial relationships.
Ashton Ellison indicated no relevant financial relationships.
Pallavi Patil indicated no relevant financial relationships.
Vani Konda: Castle – Speakers Bureau. Exact – Advisory Committee/Board Member, Consultant. Medtronic – Advisory Committee/Board Member, Consultant. Pentax – Consultant. sebela – Advisor or Review Panel Member, Consultant.
Naomi Reddy-Patel, MD1, Ashton Ellison, MBBCh2, Pallavi Patil, MD3, Vani J.A.. Konda, MD2. P0603 - Case Report: Esophagogastric Junction Outflow Obstruction Due to Infiltrative Amyloidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
