Sunday Poster Session
Category: Functional Bowel Disease
P0634 - Outcomes of Patients Infected With Clostridioides difficile With Comorbid Gastroparesis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Alexander Kaye, MD
SUNY Downstate Medical Center
Staten Island, NY
Presenting Author(s)
Alexander Kaye, MD1, Andrew Draheim, BS2, Binyamin R. Abramowitz, MD3, Daniel A. DiLeo, MD4, Bani Chander-Roland, MD, FACG5
1SUNY Downstate Medical Center, Staten Island, NY; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3SUNY Downstate Health Sciences University, New York, NY; 4Brooklyn VA Medical Center, Brooklyn, NY; 5VA NY Harbor Health System Clinical Associate Professor SUNY Downstate Health Sciences University, Brooklyn, NY
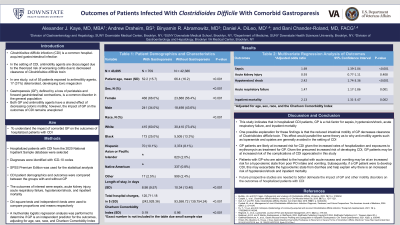
Introduction: Clostridioides difficle infection (CDI) is a common hospital acquired infection with a mortality rate of 6%. The use of antimotility agents in the setting of CDI is generally discouraged, given the theorized increased risk of more severe colitis. Gastroparesis (GP), is a common disorder among the general population characterized by loss of peristalsis and forward movement of gastric or intestinal content. Both GP and antimotility agents have a shared effect of decreasing colonic motility, however the impact of GP on the outcomes of CDI remain relatively unexplored. Our study seeks to understand the impact of comorbid GP on the outcomes of patients hospitalized with CDI.
Methods: Hospitalized adults diagnosed with CDI were selected from the 2020 National Inpatient Sample database. ICD-10 codes were used to select diagnoses. Demographic data and outcomes of CDI were compared between subgroups with and without GP. The outcomes of interest were sepsis, acute kidney injury (AKI), acute respiratory failure (ARF), hypotension/shock, and inpatient mortality. Chi-squared tests and independent t-tests were used to compare proportions and means respectively. A multivariate logistic regression analysis was used to establish if GP is an independent predictor for the outcomes after adjusting for age, sex, race, and Charlson Comorbidity Index (CCI).
Results: For the year 2020, 43,456 hospitalized adults were diagnosed with CDI. Patients with CDI and comorbid GP were younger (52.2 vs 66.4 years old, p< 0.001), more likely to be female (66.0% vs 56.4%, p< 0.001), less likely to be white (60.0% vs 73.4%, p< 0.001), and had a lower CCI (0.19 vs. 0.96, p< 0.001), had a shorter length of stay (8.98 days vs 10.34 days, p< 0.001), and a larger hospital charge ($120,711 vs $93,599, p< 0.001). GP was noted to be an independent risk factor for inpatient mortality (adjusted odds ratio (aOR) 2.13, 95% confidence interval (CI): 1.31-3.47, p=0.002), sepsis (aOR 1.69, 95% CI: 1.39-2.04, p< 0.001), hypotension/shock (aOR 2.42, 95% CI: 1.74-3.36, p< 0.001), and ARF (aOR 1.47, 95% CI: 1.17-1.86, p=0.001). GP was not a risk factor for AKI (p=0.408).
Discussion: In hospitalized adults diagnosed with CDI, GP is a risk factor for sepsis, hypotension/shock, ARF, and inpatient mortality. We hypothesize that treatment of motility disorders may improve outcomes among patients with CDI. Future prospective studies are needed to better delineate the impact of GP and other motility disorders among hospitalized patients with CDI.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alexander Kaye, MD1, Andrew Draheim, BS2, Binyamin R. Abramowitz, MD3, Daniel A. DiLeo, MD4, Bani Chander-Roland, MD, FACG5. P0634 - Outcomes of Patients Infected With Clostridioides difficile With Comorbid Gastroparesis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SUNY Downstate Medical Center, Staten Island, NY; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3SUNY Downstate Health Sciences University, New York, NY; 4Brooklyn VA Medical Center, Brooklyn, NY; 5VA NY Harbor Health System Clinical Associate Professor SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Clostridioides difficle infection (CDI) is a common hospital acquired infection with a mortality rate of 6%. The use of antimotility agents in the setting of CDI is generally discouraged, given the theorized increased risk of more severe colitis. Gastroparesis (GP), is a common disorder among the general population characterized by loss of peristalsis and forward movement of gastric or intestinal content. Both GP and antimotility agents have a shared effect of decreasing colonic motility, however the impact of GP on the outcomes of CDI remain relatively unexplored. Our study seeks to understand the impact of comorbid GP on the outcomes of patients hospitalized with CDI.
Methods: Hospitalized adults diagnosed with CDI were selected from the 2020 National Inpatient Sample database. ICD-10 codes were used to select diagnoses. Demographic data and outcomes of CDI were compared between subgroups with and without GP. The outcomes of interest were sepsis, acute kidney injury (AKI), acute respiratory failure (ARF), hypotension/shock, and inpatient mortality. Chi-squared tests and independent t-tests were used to compare proportions and means respectively. A multivariate logistic regression analysis was used to establish if GP is an independent predictor for the outcomes after adjusting for age, sex, race, and Charlson Comorbidity Index (CCI).
Results: For the year 2020, 43,456 hospitalized adults were diagnosed with CDI. Patients with CDI and comorbid GP were younger (52.2 vs 66.4 years old, p< 0.001), more likely to be female (66.0% vs 56.4%, p< 0.001), less likely to be white (60.0% vs 73.4%, p< 0.001), and had a lower CCI (0.19 vs. 0.96, p< 0.001), had a shorter length of stay (8.98 days vs 10.34 days, p< 0.001), and a larger hospital charge ($120,711 vs $93,599, p< 0.001). GP was noted to be an independent risk factor for inpatient mortality (adjusted odds ratio (aOR) 2.13, 95% confidence interval (CI): 1.31-3.47, p=0.002), sepsis (aOR 1.69, 95% CI: 1.39-2.04, p< 0.001), hypotension/shock (aOR 2.42, 95% CI: 1.74-3.36, p< 0.001), and ARF (aOR 1.47, 95% CI: 1.17-1.86, p=0.001). GP was not a risk factor for AKI (p=0.408).
Discussion: In hospitalized adults diagnosed with CDI, GP is a risk factor for sepsis, hypotension/shock, ARF, and inpatient mortality. We hypothesize that treatment of motility disorders may improve outcomes among patients with CDI. Future prospective studies are needed to better delineate the impact of GP and other motility disorders among hospitalized patients with CDI.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alexander Kaye indicated no relevant financial relationships.
Andrew Draheim indicated no relevant financial relationships.
Binyamin Abramowitz indicated no relevant financial relationships.
Daniel DiLeo indicated no relevant financial relationships.
Bani Chander-Roland indicated no relevant financial relationships.
Alexander Kaye, MD1, Andrew Draheim, BS2, Binyamin R. Abramowitz, MD3, Daniel A. DiLeo, MD4, Bani Chander-Roland, MD, FACG5. P0634 - Outcomes of Patients Infected With Clostridioides difficile With Comorbid Gastroparesis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
