Sunday Poster Session
Category: Functional Bowel Disease
P0636 - Difference in Healthcare Outcomes Between Patients With Chronic GI Conditions and Psychiatric Comorbidities
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Rakahn Haddadin, MD
MountainView Hospital
Las Vegas, NV
Presenting Author(s)
Rakahn Haddadin, MD1, Danny Aboujamra, MD2, Humzah Iqbal, MD3, George Trad, MD4, John Ryan, MD4, Emon K. Javadi, BS5, Kartika Shetty, MD1
1MountainView Hospital, Las Vegas, NV; 2Medical University of South Carolina (MUSC) Health Florence, North York, ON, Canada; 3University of California San Francisco, Fresno, CA; 4Sunrise Health GME Consortium, Las Vegas, NV; 5St. George's University School of Medicine, Anaheim, CA
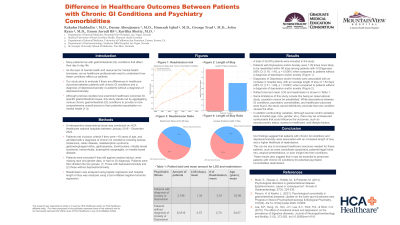
Introduction: Many patients live with gastrointestinal (GI) conditions affecting their daily lives. As the topic of mental health and resources for mental health increases, we as healthcare professionals need to understand how these conditions affect our patients. Our study aims to evaluate if there are differences in healthcare outcomes between patients with common chronic GI conditions and a diagnosis of depression/anxiety versus patients without a diagnosis of depression/anxiety. This study aims to highlight updated research findings on the impact of a diagnosis of depression or anxiety on chronic GI conditions.
Methods: A retrospective observational study was conducted on HCA national hospitals between January 2016 – December 2022. Patients met inclusion criteria if they were >18 years of age and admitted with a diagnosis of one or more of the following chronic GI conditions: lactose intolerance, celiac disease, malabsorption syndrome, gastroesophageal reflux, gastroparesis, diverticulosis, inflammatory bowel disease, hemorrhoids, eosinophilic esophagitis, irritable bowel disease. Patients were excluded if they left against medical advice, were missing race and gender, and had no GI diagnosis. Patients were then divided into a group with depression/anxiety and a group without depression/anxiety.
Results: A total of 34,876 patients were included in the study. Among patients with chronic GI diagnoses at the index encounter, those with depression and/or anxiety were 1.29 times more likely to be readmitted within 90 days when controlling for age, race, gender, diabetes, hypertension, and hyperlipidemia (95% CI [1.18, 1.41], p< .001). Diagnoses of depression and/or anxiety were associated with a 1.50 increase in the count of days in the hospital (95% CI [1.31, 1.60], p < .0001). Table 1 shows further findings from the data set.
Discussion: Our findings suggest that patients with chronic GI conditions and depression/anxiety were associated with an increased length of stay and a higher likelihood of readmission. This can be due to increased healthcare resources needed for these patients, such as extra consultants (psychiatry, potential legal holds, etc), atypical presentations, or poor insight into their conditions. These results also suggest that it may be essential to prescreen patients with chronic GI conditions for potential psychiatric comorbidities to avoid the increase in healthcare resources, especially given the high likelihood of comorbidity with GI conditions and depression/anxiety.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rakahn Haddadin, MD1, Danny Aboujamra, MD2, Humzah Iqbal, MD3, George Trad, MD4, John Ryan, MD4, Emon K. Javadi, BS5, Kartika Shetty, MD1. P0636 - Difference in Healthcare Outcomes Between Patients With Chronic GI Conditions and Psychiatric Comorbidities, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1MountainView Hospital, Las Vegas, NV; 2Medical University of South Carolina (MUSC) Health Florence, North York, ON, Canada; 3University of California San Francisco, Fresno, CA; 4Sunrise Health GME Consortium, Las Vegas, NV; 5St. George's University School of Medicine, Anaheim, CA
Introduction: Many patients live with gastrointestinal (GI) conditions affecting their daily lives. As the topic of mental health and resources for mental health increases, we as healthcare professionals need to understand how these conditions affect our patients. Our study aims to evaluate if there are differences in healthcare outcomes between patients with common chronic GI conditions and a diagnosis of depression/anxiety versus patients without a diagnosis of depression/anxiety. This study aims to highlight updated research findings on the impact of a diagnosis of depression or anxiety on chronic GI conditions.
Methods: A retrospective observational study was conducted on HCA national hospitals between January 2016 – December 2022. Patients met inclusion criteria if they were >18 years of age and admitted with a diagnosis of one or more of the following chronic GI conditions: lactose intolerance, celiac disease, malabsorption syndrome, gastroesophageal reflux, gastroparesis, diverticulosis, inflammatory bowel disease, hemorrhoids, eosinophilic esophagitis, irritable bowel disease. Patients were excluded if they left against medical advice, were missing race and gender, and had no GI diagnosis. Patients were then divided into a group with depression/anxiety and a group without depression/anxiety.
Results: A total of 34,876 patients were included in the study. Among patients with chronic GI diagnoses at the index encounter, those with depression and/or anxiety were 1.29 times more likely to be readmitted within 90 days when controlling for age, race, gender, diabetes, hypertension, and hyperlipidemia (95% CI [1.18, 1.41], p< .001). Diagnoses of depression and/or anxiety were associated with a 1.50 increase in the count of days in the hospital (95% CI [1.31, 1.60], p < .0001). Table 1 shows further findings from the data set.
Discussion: Our findings suggest that patients with chronic GI conditions and depression/anxiety were associated with an increased length of stay and a higher likelihood of readmission. This can be due to increased healthcare resources needed for these patients, such as extra consultants (psychiatry, potential legal holds, etc), atypical presentations, or poor insight into their conditions. These results also suggest that it may be essential to prescreen patients with chronic GI conditions for potential psychiatric comorbidities to avoid the increase in healthcare resources, especially given the high likelihood of comorbidity with GI conditions and depression/anxiety.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Rakahn Haddadin indicated no relevant financial relationships.
Danny Aboujamra indicated no relevant financial relationships.
Humzah Iqbal indicated no relevant financial relationships.
George Trad indicated no relevant financial relationships.
John Ryan indicated no relevant financial relationships.
Emon Javadi indicated no relevant financial relationships.
Kartika Shetty indicated no relevant financial relationships.
Rakahn Haddadin, MD1, Danny Aboujamra, MD2, Humzah Iqbal, MD3, George Trad, MD4, John Ryan, MD4, Emon K. Javadi, BS5, Kartika Shetty, MD1. P0636 - Difference in Healthcare Outcomes Between Patients With Chronic GI Conditions and Psychiatric Comorbidities, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
