Sunday Poster Session
Category: Functional Bowel Disease
P0643 - Gastroparesis is an Independent Risk Factor for Hospitalization During Emergency Department Visits for Congestive Heart Failure
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

William Hirsch, MD
University of Minnesota Medical Center
Minneapolis, MN
Presenting Author(s)
William Hirsch, MD1, Mohammad Bilal, MD2, Byron Vaughn, MD, MS1
1University of Minnesota Medical Center, Minneapolis, MN; 2University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Patients with both gastroparesis (GP) and congestive heart failure (CHF) demonstrate autonomic dysfunction with decreased vagal tone and an overactive sympathetic nervous system. Gastric emptying rate is reduced in CHF due to increased sympathetic and reduced parasympathetic activity. Exacerbation of one condition may lead to an exacerbation of the other. Therefore, we investigated whether patients with GP presenting to the emergency department (ED) for CHF were more likely to be hospitalized than those without GP.
Methods: Data were obtained from the Nationwide Emergency Department Sample (NEDS) and National Inpatient Sample (NIS) from the Healthcare Cost and Utilization Project. These data are weighted to provide an annual representative sample of all ED visits in the US. International Classification of Diseases, 9th Revision codes were used to identify conditions of interest. Statistical analysis was completed using R from the 2006 and 2014 NEDS and NIS databases.
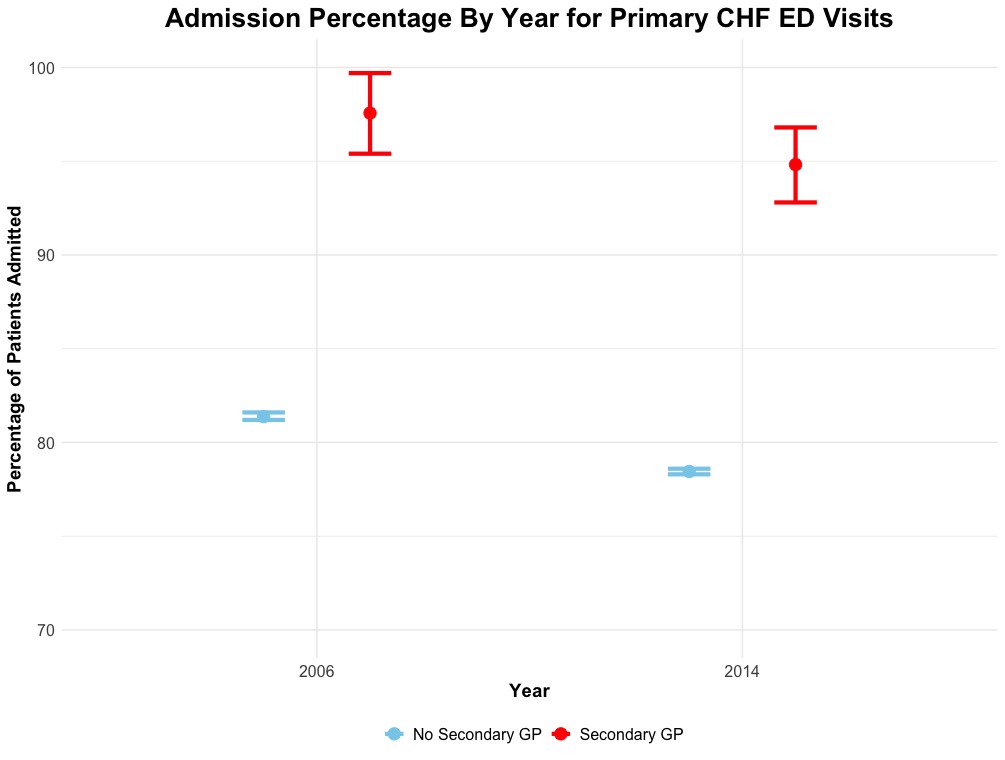
Results: In 2006, 4,028 (97.6%) of patients presenting to the ED with a primary diagnosis of CHF and a secondary diagnosis of GP were hospitalized compared to 864,364 (81.3%) with CHF without GP (P = < 0.001) (Figure 1). In 2014, 4,491 (94.8%) of patients with CHF and secondary GP were hospitalized compared to 842,707 (78.5%) without secondary GP (P = < 0.001) (Figure 1). In 2006, patients with CHF and secondary GP had a longer length of stay compared to those without GP (6.20 (5.70 – 6.60) vs. 5.28 (5.25 – 5.30), P = < 0.001). This was also true in 2014 (6.30 (5.90 – 6.70) vs. 5.16 (5.14 – 5.18), P = < 0.001). Table 1 shows the effect of GP on CHF admission controlled for select secondary diagnoses and number of secondary diagnoses divided into tertiles. When controlling for secondary diagnoses, GP was independently associated with a higher risk of hospitalization in 2006 and 2014. The magnitude of the effect of GP varied based on medical complexity (defined by number of secondary diagnoses coded). The effect of GP on CHF admission was greatest for the 2nd tertile of number of secondary diagnoses in both 2006 (8 – 10 diagnoses) and 2014 (11 - 17 diagnoses).
Discussion: GP is an independent predictor of hospitalization in patients presenting to the ED with CHF. This may be due to the overlapping pathophysiology in GP and CHF related to autonomic dysfunction. Further research is needed to elucidate the pathophysiologic mechanisms of this interaction and develop strategies to improve outpatient care in this unique population.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
William Hirsch, MD1, Mohammad Bilal, MD2, Byron Vaughn, MD, MS1. P0643 - Gastroparesis is an Independent Risk Factor for Hospitalization During Emergency Department Visits for Congestive Heart Failure, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota Medical Center, Minneapolis, MN; 2University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Patients with both gastroparesis (GP) and congestive heart failure (CHF) demonstrate autonomic dysfunction with decreased vagal tone and an overactive sympathetic nervous system. Gastric emptying rate is reduced in CHF due to increased sympathetic and reduced parasympathetic activity. Exacerbation of one condition may lead to an exacerbation of the other. Therefore, we investigated whether patients with GP presenting to the emergency department (ED) for CHF were more likely to be hospitalized than those without GP.
Methods: Data were obtained from the Nationwide Emergency Department Sample (NEDS) and National Inpatient Sample (NIS) from the Healthcare Cost and Utilization Project. These data are weighted to provide an annual representative sample of all ED visits in the US. International Classification of Diseases, 9th Revision codes were used to identify conditions of interest. Statistical analysis was completed using R from the 2006 and 2014 NEDS and NIS databases.
Results: In 2006, 4,028 (97.6%) of patients presenting to the ED with a primary diagnosis of CHF and a secondary diagnosis of GP were hospitalized compared to 864,364 (81.3%) with CHF without GP (P = < 0.001) (Figure 1). In 2014, 4,491 (94.8%) of patients with CHF and secondary GP were hospitalized compared to 842,707 (78.5%) without secondary GP (P = < 0.001) (Figure 1). In 2006, patients with CHF and secondary GP had a longer length of stay compared to those without GP (6.20 (5.70 – 6.60) vs. 5.28 (5.25 – 5.30), P = < 0.001). This was also true in 2014 (6.30 (5.90 – 6.70) vs. 5.16 (5.14 – 5.18), P = < 0.001). Table 1 shows the effect of GP on CHF admission controlled for select secondary diagnoses and number of secondary diagnoses divided into tertiles. When controlling for secondary diagnoses, GP was independently associated with a higher risk of hospitalization in 2006 and 2014. The magnitude of the effect of GP varied based on medical complexity (defined by number of secondary diagnoses coded). The effect of GP on CHF admission was greatest for the 2nd tertile of number of secondary diagnoses in both 2006 (8 – 10 diagnoses) and 2014 (11 - 17 diagnoses).
Discussion: GP is an independent predictor of hospitalization in patients presenting to the ED with CHF. This may be due to the overlapping pathophysiology in GP and CHF related to autonomic dysfunction. Further research is needed to elucidate the pathophysiologic mechanisms of this interaction and develop strategies to improve outpatient care in this unique population.
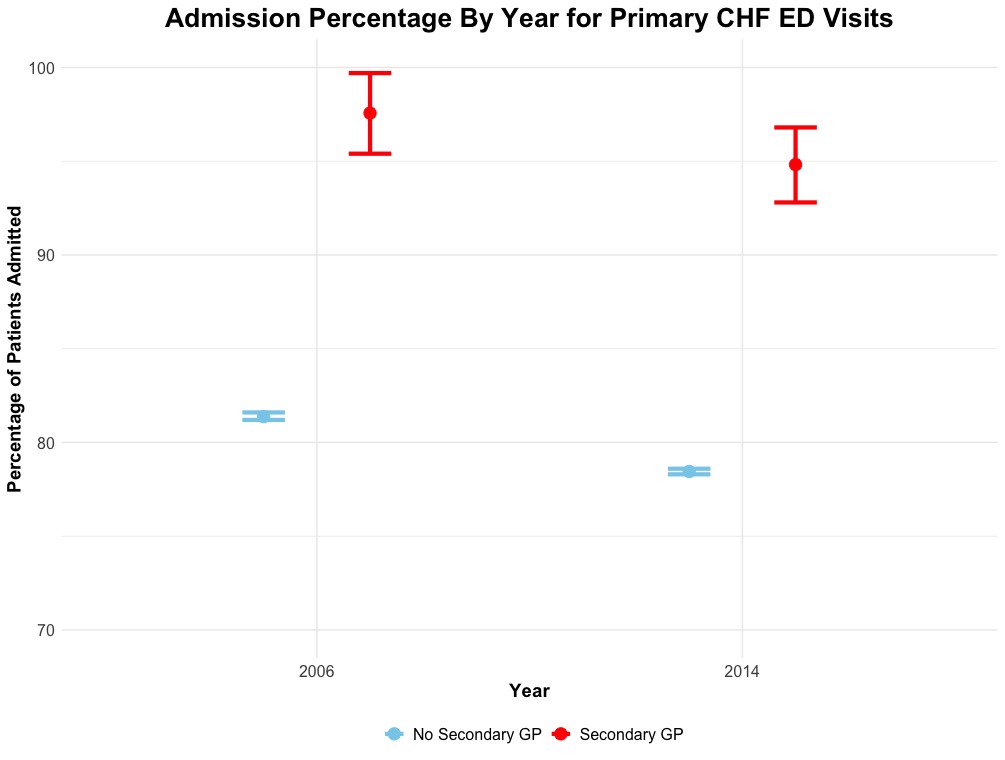
Figure: Figure 1: Percentage of Patients with Congestive Heart Failure Admitted to the Hospital By Year and Presence of a Secondary Diagnosis of Gastroparesis
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
William Hirsch indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Speakers Bureau.
Byron Vaughn: HealthDelegates – Consultant.
William Hirsch, MD1, Mohammad Bilal, MD2, Byron Vaughn, MD, MS1. P0643 - Gastroparesis is an Independent Risk Factor for Hospitalization During Emergency Department Visits for Congestive Heart Failure, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
