Sunday Poster Session
Category: General Endoscopy
P0689 - Rapunzel, Rapunzel Let Down Thy Hair: Streptococcus Intermedius Liver Abscess Secondary to an Indwelling, Transmural, Duodenal Suture
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Marisa-Nicole Zayat, MD
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Marisa-Nicole Zayat, MD1, Micah Vander Griend, MPH1, Diala Merheb, MD1, Mahmoud Mahdi, MD1, Estephan Zayat, MD2
1University of Kansas School of Medicine, Wichita, KS; 2Kansas Gastroenterology and Endoscopy, LLC, Wichita, KS
Introduction: Liver abscesses develop from direct trauma or dissemination via portal circulation. E.coli, Klebsiella, Streptococcus, Staphylococcus, and anaerobes are common bacterial culprits.
Case Description/Methods: A 71-year-old female was admitted with suspected urosepsis after failing outpatient treatment. Five years prior, she underwent a cholecystectomy and a NSAID-induced perforated peptic ulcer repair requiring an omental patch. Urine and blood cultures were negative. She was discharged after completing a five day course of ceftriaxone. Outpatient GI was consulted for an incidental 4.9 x 4.0 cm hepatic mass found on CT.
Follow-up MRI three weeks post-discharge demonstrated a heterogeneous, multilobulated, partially cystic posterior right hepatic lesion measuring 6.5 x 6.7 x 4.8 cm. MRCP was negative. Liver biopsy demonstrated acute and chronic inflammation with fibrosis. Liver tissue cultures grew Streptococcus intermedius. The patient re-presented to the hospital for post-biopsy pain, and an empiric five day course of Zosyn was started. At discharge, the patient was transitioned to a two week course of Augmentin, then a 13 week course of amoxicillin.
Repeat CT two months following her MRI showed a significant reduction in the abscess size, down to 1.6 cm. At three months, there was near complete resolution of the abscess.
To determine the infection’s origin, a thorough workup was completed. TEE was negative for valvular vegetation. Intraluminal sources were assessed via endoscopy. EGD one month after the termination of antibiotic therapy revealed two silk sutures in the second portion of the duodenum. The location prevented endoscopic suture scissors from opening. The sutures were removed with forceps with a little traction. No evidence of perforation or bleeding were noted. Colonoscopy revealed one 10 mm flat polyp in the ascending colon, consistent with a sessile serrated adenoma on biopsy. Repeat colonoscopy in 6 months was negative. The patient did not experience any abscess recurrences to date.
Discussion: Strep. intermedius is predisposed to forming abscesses. It comprises part of the upper GI flora. Its most common origins are venous splanchnic drainage from GI sources, biliary obstruction, or hematogenous spread from endocarditis. Much like how Rapunzel’s hair allows access to her tower, we suspect that the bacteria gained extraluminal access via the silk sutures. This case novelly highlights how remnant transmural duodenal sutures should be considered for cryptogenic liver abscesses.
Disclosures:
Marisa-Nicole Zayat, MD1, Micah Vander Griend, MPH1, Diala Merheb, MD1, Mahmoud Mahdi, MD1, Estephan Zayat, MD2. P0689 - Rapunzel, Rapunzel Let Down Thy Hair: Streptococcus Intermedius Liver Abscess Secondary to an Indwelling, Transmural, Duodenal Suture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kansas School of Medicine, Wichita, KS; 2Kansas Gastroenterology and Endoscopy, LLC, Wichita, KS
Introduction: Liver abscesses develop from direct trauma or dissemination via portal circulation. E.coli, Klebsiella, Streptococcus, Staphylococcus, and anaerobes are common bacterial culprits.
Case Description/Methods: A 71-year-old female was admitted with suspected urosepsis after failing outpatient treatment. Five years prior, she underwent a cholecystectomy and a NSAID-induced perforated peptic ulcer repair requiring an omental patch. Urine and blood cultures were negative. She was discharged after completing a five day course of ceftriaxone. Outpatient GI was consulted for an incidental 4.9 x 4.0 cm hepatic mass found on CT.
Follow-up MRI three weeks post-discharge demonstrated a heterogeneous, multilobulated, partially cystic posterior right hepatic lesion measuring 6.5 x 6.7 x 4.8 cm. MRCP was negative. Liver biopsy demonstrated acute and chronic inflammation with fibrosis. Liver tissue cultures grew Streptococcus intermedius. The patient re-presented to the hospital for post-biopsy pain, and an empiric five day course of Zosyn was started. At discharge, the patient was transitioned to a two week course of Augmentin, then a 13 week course of amoxicillin.
Repeat CT two months following her MRI showed a significant reduction in the abscess size, down to 1.6 cm. At three months, there was near complete resolution of the abscess.
To determine the infection’s origin, a thorough workup was completed. TEE was negative for valvular vegetation. Intraluminal sources were assessed via endoscopy. EGD one month after the termination of antibiotic therapy revealed two silk sutures in the second portion of the duodenum. The location prevented endoscopic suture scissors from opening. The sutures were removed with forceps with a little traction. No evidence of perforation or bleeding were noted. Colonoscopy revealed one 10 mm flat polyp in the ascending colon, consistent with a sessile serrated adenoma on biopsy. Repeat colonoscopy in 6 months was negative. The patient did not experience any abscess recurrences to date.
Discussion: Strep. intermedius is predisposed to forming abscesses. It comprises part of the upper GI flora. Its most common origins are venous splanchnic drainage from GI sources, biliary obstruction, or hematogenous spread from endocarditis. Much like how Rapunzel’s hair allows access to her tower, we suspect that the bacteria gained extraluminal access via the silk sutures. This case novelly highlights how remnant transmural duodenal sutures should be considered for cryptogenic liver abscesses.
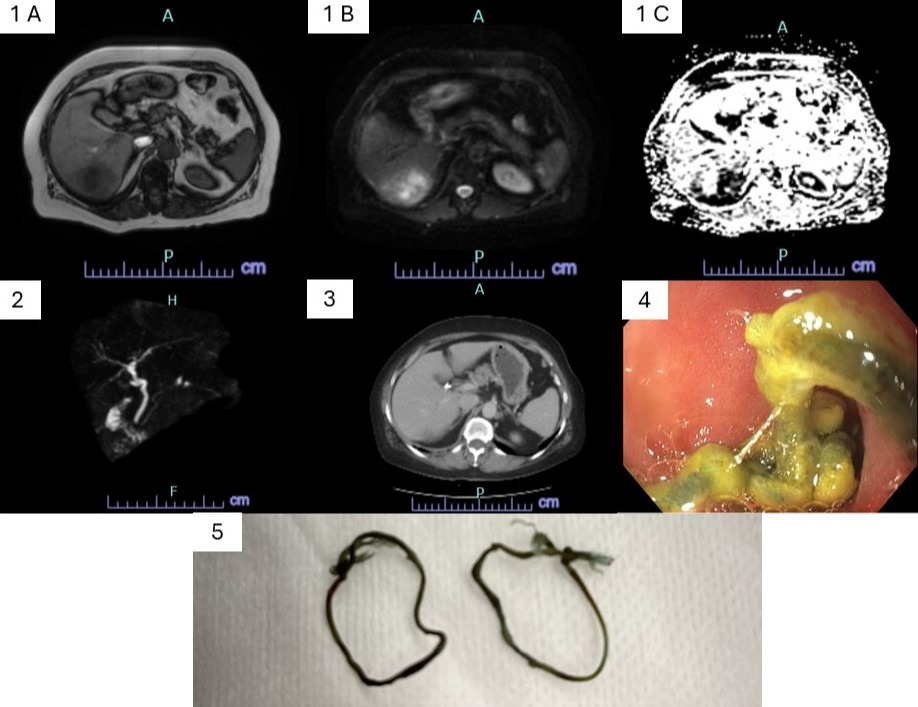
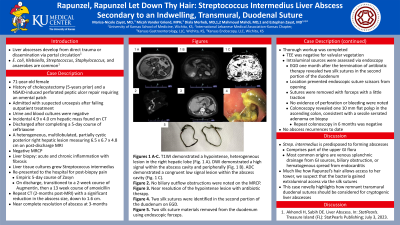
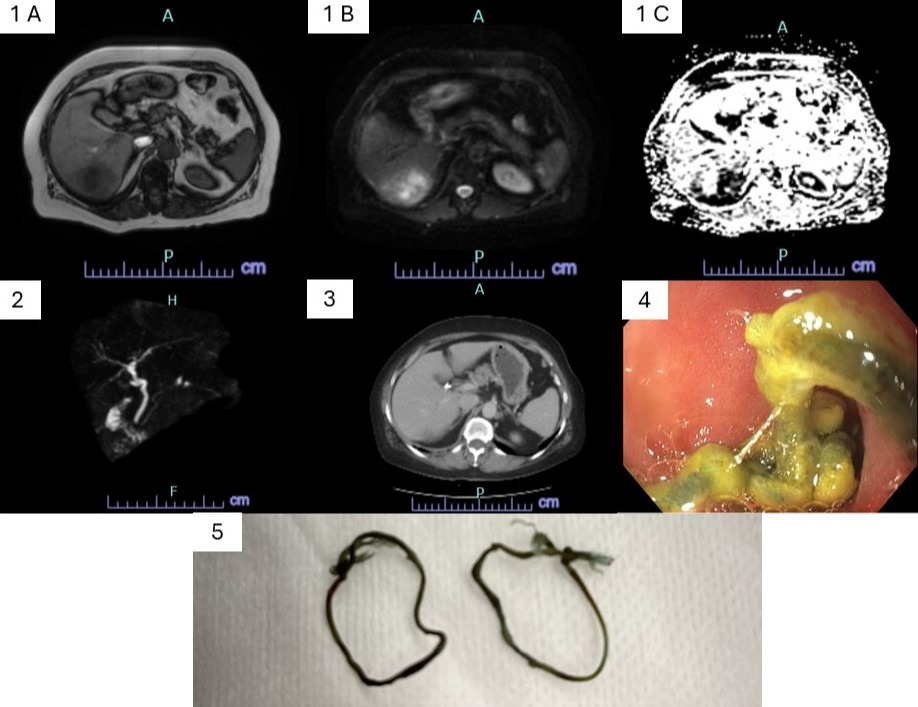
Figure: Figures 1 A-C. T1WI demonstrated a hypointense, heterogenous lesion in the right hepatic lobe (Fig. 1 A). DWI demonstrated a high signal within the abscess cavity and peripherally (Fig. 1 B). ADC demonstrated a congruent low signal lesion within the abscess cavity (Fig. 1 C).
Figure 2. No biliary outflow obstructions were noted on the MRCP.
Figure 3. Near resolution of the hypointense lesion with antibiotic therapy.
Figure 4. Two silk sutures were identified in the second portion of the duodenum on EGD.
Figure 5. Two silk suture materials removed from the duodenum using endoscopic forceps.
Figure 2. No biliary outflow obstructions were noted on the MRCP.
Figure 3. Near resolution of the hypointense lesion with antibiotic therapy.
Figure 4. Two silk sutures were identified in the second portion of the duodenum on EGD.
Figure 5. Two silk suture materials removed from the duodenum using endoscopic forceps.
Disclosures:
Marisa-Nicole Zayat indicated no relevant financial relationships.
Micah Vander Griend indicated no relevant financial relationships.
Diala Merheb indicated no relevant financial relationships.
Mahmoud Mahdi indicated no relevant financial relationships.
Estephan Zayat indicated no relevant financial relationships.
Marisa-Nicole Zayat, MD1, Micah Vander Griend, MPH1, Diala Merheb, MD1, Mahmoud Mahdi, MD1, Estephan Zayat, MD2. P0689 - Rapunzel, Rapunzel Let Down Thy Hair: Streptococcus Intermedius Liver Abscess Secondary to an Indwelling, Transmural, Duodenal Suture, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
