Sunday Poster Session
Category: General Endoscopy
P0690 - EBV-Positive Plasmablastic Lymphoma of the Terminal Ileum on Routine Screening Colonoscopy: Rare Case Report
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Saad Nadeem, MBA
Texas A&M School of Medicine, TX
Presenting Author(s)
Saad Nadeem, MBA1, Syed F. Jafri, MD2, Anish Meerasahib, MD3, Sa Wang, MD4, Ali Totonchian, MD5, Mark Podberezin, MD6
1Texas A&M School of Medicine, Webster, TX; 2Texas Digestive Disease Consultants, Houston, TX; 3Texas Oncology, Webster, TX; 4MD Anderson Cancer Center, Houston, TX; 5Laredo Medical Center, Houston, TX; 6GI Alliance, Dallas, TX
Introduction: Plasmablastic lymphoma (PBL), an uncommon and severe B-cell lymphoma, is often linked to Epstein-Barr virus (EBV) infection and generally compromised immune systems. PBL is rarely seen in extra-oral locations and is typically observed in the oral cavity of HIV-positive individuals. This case report describes a rare occurrence of PBL in the terminal ileum of an immunocompetent asymptomatic patient during a routine screening colonoscopy. Rarely does one witness this presentation in clinical practice. This oddity emphasizes the difficulties in diagnosing and the need for careful management in such unusual presentations.
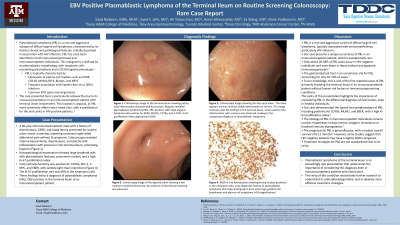
Case Description/Methods: A 66-year-old white man with obesity, diverticulosis, and GERD came in for a regular colon cancer screening. He mentioned occasional right abdominal pain but denied fever, night sweats, weight loss, or change in bowel habits. The patient had no history of myeloma or immunodeficiency. Procedure findings included internal hemorrhoids, diverticulosis, and patchy ileitis with biopsy of the terminal ileum consistent with plasmablastic lymphoma, EBV positive. Biopsies reveal ileal mucosa with infiltration by large atypical lymphoid cells which are positive for EBER, MUM1, CD79a, C-MYC, and show lambda light chain restriction by kappa and lambda ISH. Ki-67 proliferation index approaches 100%. Adjacent reactive lymphoid aggregates like CD20, CD3, CD5, BCL-2, and CD23 were positive. Clinical and radiologic correlations were part of additional diagnostic workup to determine the extent of the illness and rule out other likely causes. A hematologist-oncologist was consulted for the patient's further care, which included intensive chemotherapy.
Discussion: This case highlights the challenges of diagnosing PBL, even for patients who are immunocompetent. We were able to confirm the diagnosis by combining several tests using histology, immunohistochemistry, and the results of the colonoscopy. While aggressive chemotherapy is the standard treatment, the outlook for patients with PBL often remains poor due to the fast-growing nature of the cancer. This case adds valuable information to the limited research on PBL in the digestive system. The lessons learned from this case study underline the importance of a quality colonoscopy including terminal ileum evaluation to detect the possibility of serious illness, even in patients without the usual risk factors.
Disclosures:
Saad Nadeem, MBA1, Syed F. Jafri, MD2, Anish Meerasahib, MD3, Sa Wang, MD4, Ali Totonchian, MD5, Mark Podberezin, MD6. P0690 - EBV-Positive Plasmablastic Lymphoma of the Terminal Ileum on Routine Screening Colonoscopy: Rare Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Texas A&M School of Medicine, Webster, TX; 2Texas Digestive Disease Consultants, Houston, TX; 3Texas Oncology, Webster, TX; 4MD Anderson Cancer Center, Houston, TX; 5Laredo Medical Center, Houston, TX; 6GI Alliance, Dallas, TX
Introduction: Plasmablastic lymphoma (PBL), an uncommon and severe B-cell lymphoma, is often linked to Epstein-Barr virus (EBV) infection and generally compromised immune systems. PBL is rarely seen in extra-oral locations and is typically observed in the oral cavity of HIV-positive individuals. This case report describes a rare occurrence of PBL in the terminal ileum of an immunocompetent asymptomatic patient during a routine screening colonoscopy. Rarely does one witness this presentation in clinical practice. This oddity emphasizes the difficulties in diagnosing and the need for careful management in such unusual presentations.
Case Description/Methods: A 66-year-old white man with obesity, diverticulosis, and GERD came in for a regular colon cancer screening. He mentioned occasional right abdominal pain but denied fever, night sweats, weight loss, or change in bowel habits. The patient had no history of myeloma or immunodeficiency. Procedure findings included internal hemorrhoids, diverticulosis, and patchy ileitis with biopsy of the terminal ileum consistent with plasmablastic lymphoma, EBV positive. Biopsies reveal ileal mucosa with infiltration by large atypical lymphoid cells which are positive for EBER, MUM1, CD79a, C-MYC, and show lambda light chain restriction by kappa and lambda ISH. Ki-67 proliferation index approaches 100%. Adjacent reactive lymphoid aggregates like CD20, CD3, CD5, BCL-2, and CD23 were positive. Clinical and radiologic correlations were part of additional diagnostic workup to determine the extent of the illness and rule out other likely causes. A hematologist-oncologist was consulted for the patient's further care, which included intensive chemotherapy.
Discussion: This case highlights the challenges of diagnosing PBL, even for patients who are immunocompetent. We were able to confirm the diagnosis by combining several tests using histology, immunohistochemistry, and the results of the colonoscopy. While aggressive chemotherapy is the standard treatment, the outlook for patients with PBL often remains poor due to the fast-growing nature of the cancer. This case adds valuable information to the limited research on PBL in the digestive system. The lessons learned from this case study underline the importance of a quality colonoscopy including terminal ileum evaluation to detect the possibility of serious illness, even in patients without the usual risk factors.
Disclosures:
Saad Nadeem indicated no relevant financial relationships.
Syed Jafri indicated no relevant financial relationships.
Anish Meerasahib indicated no relevant financial relationships.
Sa Wang indicated no relevant financial relationships.
Ali Totonchian indicated no relevant financial relationships.
Mark Podberezin indicated no relevant financial relationships.
Saad Nadeem, MBA1, Syed F. Jafri, MD2, Anish Meerasahib, MD3, Sa Wang, MD4, Ali Totonchian, MD5, Mark Podberezin, MD6. P0690 - EBV-Positive Plasmablastic Lymphoma of the Terminal Ileum on Routine Screening Colonoscopy: Rare Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
