Sunday Poster Session
Category: General Endoscopy
P0696 - Duodenal Endovascular Stent Protrusion Without Gastrointestinal Bleeding
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- MF
Maham Farshidpour, MD
Loma Linda University Health
Loma Linda, CA
Presenting Author(s)
Maham Farshidpour, MD, Harold J. Duarte, MD, Nour Parsa, MD
Loma Linda University Health, Loma Linda, CA
Introduction: An aortoenteric fistula (AEF) is defined as a communication of the aortic graft with an adjacent loop of bowel. Primary AEF occurs in patient’s without any history of aortic surgery or trauma to explain fistula formation. Secondary AEF is a rare complication of aortic surgical intervention such as abdominal aortic aneurysm repair. AEF has a high mortality rate, requiring prompt diagnosis and emergent surgical intervention. We report a case of a patient with secondary aortoenteric fistula complicated by sepsis and anemia.
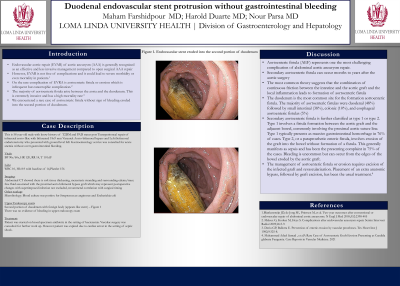
Case Description/Methods: We describe a case of AEF without evidence of a herald bleed or overt gastrointestinal bleeding. The patient was a 58-year-old male who presented with sepsis and acute anemia without any signs of overt gastrointestinal hemorrhage. Empiric antibiotics were started due to sepsis and bacteremia, with blood cultures positive for Streptococcus anginosus and Escherichia coli. As part of his anemia workup, he underwent an upper endoscopy which revealed an erosion of the aortic graft into the second portion of the duodenum without evidence of bleeding. Unfortunately, this patient’s hospital course was complicated by worsening hypotension likely due to septic shock, and eventually the patient expired.
Discussion: The duodenum is the most common site for the formation aortoenteric fistula. Secondary AEF is classified as type 1 or type 2. Type 1, also called true AEF or graft enteric fistula, typically presents as massive gastrointestinal hemorrhage in 76% of cases as it involves communication of aortic graft lumen and bowel lumen. Type 2, also called para-prosthetic enteric fistula, generally manifests as sepsis as there is no direct communication between the graft lumen and the bowel lumen. In our case, the patient had a type 2 secondary AEF. In these types of cases, bleeding can occur from the area of the bowel wall that has been eroded by the intact graft. This is suspected to have led to occult bleeding and anemia in our patient. A low threshold for performing endoscopic evaluation because of worsening anemia helped establish the diagnosis of AEF in our patient’s case. Management involves emergency surgical intervention with excision of any infected tissue, repair of the damaged portion of the aorta/graft and intestinal resection of the affected segment. Our case is a reminder of the importance of thorough history taking and consideration of rare but deadly differential diagnoses in the setting of non-classic patient presentations.
Disclosures:
Maham Farshidpour, MD, Harold J. Duarte, MD, Nour Parsa, MD. P0696 - Duodenal Endovascular Stent Protrusion Without Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Loma Linda University Health, Loma Linda, CA
Introduction: An aortoenteric fistula (AEF) is defined as a communication of the aortic graft with an adjacent loop of bowel. Primary AEF occurs in patient’s without any history of aortic surgery or trauma to explain fistula formation. Secondary AEF is a rare complication of aortic surgical intervention such as abdominal aortic aneurysm repair. AEF has a high mortality rate, requiring prompt diagnosis and emergent surgical intervention. We report a case of a patient with secondary aortoenteric fistula complicated by sepsis and anemia.
Case Description/Methods: We describe a case of AEF without evidence of a herald bleed or overt gastrointestinal bleeding. The patient was a 58-year-old male who presented with sepsis and acute anemia without any signs of overt gastrointestinal hemorrhage. Empiric antibiotics were started due to sepsis and bacteremia, with blood cultures positive for Streptococcus anginosus and Escherichia coli. As part of his anemia workup, he underwent an upper endoscopy which revealed an erosion of the aortic graft into the second portion of the duodenum without evidence of bleeding. Unfortunately, this patient’s hospital course was complicated by worsening hypotension likely due to septic shock, and eventually the patient expired.
Discussion: The duodenum is the most common site for the formation aortoenteric fistula. Secondary AEF is classified as type 1 or type 2. Type 1, also called true AEF or graft enteric fistula, typically presents as massive gastrointestinal hemorrhage in 76% of cases as it involves communication of aortic graft lumen and bowel lumen. Type 2, also called para-prosthetic enteric fistula, generally manifests as sepsis as there is no direct communication between the graft lumen and the bowel lumen. In our case, the patient had a type 2 secondary AEF. In these types of cases, bleeding can occur from the area of the bowel wall that has been eroded by the intact graft. This is suspected to have led to occult bleeding and anemia in our patient. A low threshold for performing endoscopic evaluation because of worsening anemia helped establish the diagnosis of AEF in our patient’s case. Management involves emergency surgical intervention with excision of any infected tissue, repair of the damaged portion of the aorta/graft and intestinal resection of the affected segment. Our case is a reminder of the importance of thorough history taking and consideration of rare but deadly differential diagnoses in the setting of non-classic patient presentations.
Disclosures:
Maham Farshidpour indicated no relevant financial relationships.
Harold Duarte indicated no relevant financial relationships.
Nour Parsa indicated no relevant financial relationships.
Maham Farshidpour, MD, Harold J. Duarte, MD, Nour Parsa, MD. P0696 - Duodenal Endovascular Stent Protrusion Without Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
