Sunday Poster Session
Category: General Endoscopy
P0699 - Underwater Endoscopic Mucosal Resection of Rectal Neuroendocrine Tumors – A Case Series of an Innovative Endoscopic Approach
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- FM
Francisco Mendes, MD
Centro Hospitalar Universitário de São João
Porto, Porto, Portugal
Presenting Author(s)
Francisco Mendes, MD1, Rui Morais, MD1, Irene Gullo, MD, PhD2, Guilherme Macedo, MD, PhD, FACG1
1Centro Hospitalar Universitário de São João, Porto, Porto, Portugal; 2Centro Hospitalar Universitário São João, Porto, Porto, Portugal
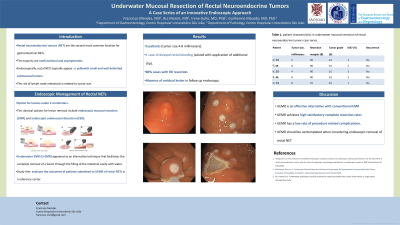
Introduction: Neuroendocrine neoplasms originate from neuroendocrine cells and peptidergic neurons. Rectal neuroendocrine tumors (NETs) are the second most common gastrointestinal NETs. Most of these are nonfunctional and asymptomatic although pain, blood loss and perianal discomfort can occur in larger lesions. Endoscopically, rectal NETs typically appear as yellowish small and well-delimited submucosal lesions. The current guidelines consider endoscopic resection as an option for rectal NETs smaller than 2 centimeters. The classical options for lesion removal include endoscopic mucosal resection (EMR), with higher risk of incomplete resection, and endoscopic submucosal dissection (ESD), with an increased risk of complications (namely bleeding and perforation). In this setting, underwater endoscopic mucosal resection (UEMR) appeared as an alternative that facilitates the complete removal of a lesion through the filling of the intestinal cavity with water. The present study aimed to evaluate the outcomes of patients submitted to UEMR of rectal NETs in a reference center.
Case Description/Methods: A total of 5 patients underwent UEMR for a rectal NETs. 3 patients had a tumor from the proximal rectum and 2 patients from the distal rectum. The tumor size ranged between 4 and 8 millimeters.
After marking the lesion borders, the entire rectal cavity was filled with saline and UEMR was performed. The lesion scar was closed with endoscopic clips in all cases. In a single case, delayed rectal bleeding was observed 3 days after procedure, solved with application of an additional endoscopic clip, without the need of inpatient management. No other complications were reported.
A R0 resection was observed in 80% of the cases. In a single case a positive basolateral margin was observed. However, after performance of a second UEMR in the scar (where no endoscopic evidence of residual lesion was found), there was absence of lesion in the histopathological sample. All the tumors had a G1 grade in the WHO 2019 Classification for Neuroendocrine Tumors, with a Ki-67 index ranging between 1 and 3%.
In all the cases there was absence of residual lesion or recurrence in the follow up endoscopy.
Discussion: This case series showcases UEMR as an effective alternative to conventional EMR, achieving high satisfactory complete resection rates, while having a low rate of procedure related complications. Therefore, UEMR should be contemplated when considering an endoscopic removal for rectal neuroendocrine neoplasms.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Francisco Mendes, MD1, Rui Morais, MD1, Irene Gullo, MD, PhD2, Guilherme Macedo, MD, PhD, FACG1. P0699 - Underwater Endoscopic Mucosal Resection of Rectal Neuroendocrine Tumors – A Case Series of an Innovative Endoscopic Approach, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Centro Hospitalar Universitário de São João, Porto, Porto, Portugal; 2Centro Hospitalar Universitário São João, Porto, Porto, Portugal
Introduction: Neuroendocrine neoplasms originate from neuroendocrine cells and peptidergic neurons. Rectal neuroendocrine tumors (NETs) are the second most common gastrointestinal NETs. Most of these are nonfunctional and asymptomatic although pain, blood loss and perianal discomfort can occur in larger lesions. Endoscopically, rectal NETs typically appear as yellowish small and well-delimited submucosal lesions. The current guidelines consider endoscopic resection as an option for rectal NETs smaller than 2 centimeters. The classical options for lesion removal include endoscopic mucosal resection (EMR), with higher risk of incomplete resection, and endoscopic submucosal dissection (ESD), with an increased risk of complications (namely bleeding and perforation). In this setting, underwater endoscopic mucosal resection (UEMR) appeared as an alternative that facilitates the complete removal of a lesion through the filling of the intestinal cavity with water. The present study aimed to evaluate the outcomes of patients submitted to UEMR of rectal NETs in a reference center.
Case Description/Methods: A total of 5 patients underwent UEMR for a rectal NETs. 3 patients had a tumor from the proximal rectum and 2 patients from the distal rectum. The tumor size ranged between 4 and 8 millimeters.
After marking the lesion borders, the entire rectal cavity was filled with saline and UEMR was performed. The lesion scar was closed with endoscopic clips in all cases. In a single case, delayed rectal bleeding was observed 3 days after procedure, solved with application of an additional endoscopic clip, without the need of inpatient management. No other complications were reported.
A R0 resection was observed in 80% of the cases. In a single case a positive basolateral margin was observed. However, after performance of a second UEMR in the scar (where no endoscopic evidence of residual lesion was found), there was absence of lesion in the histopathological sample. All the tumors had a G1 grade in the WHO 2019 Classification for Neuroendocrine Tumors, with a Ki-67 index ranging between 1 and 3%.
In all the cases there was absence of residual lesion or recurrence in the follow up endoscopy.
Discussion: This case series showcases UEMR as an effective alternative to conventional EMR, achieving high satisfactory complete resection rates, while having a low rate of procedure related complications. Therefore, UEMR should be contemplated when considering an endoscopic removal for rectal neuroendocrine neoplasms.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Francisco Mendes indicated no relevant financial relationships.
Rui Morais indicated no relevant financial relationships.
Irene Gullo indicated no relevant financial relationships.
Guilherme Macedo indicated no relevant financial relationships.
Francisco Mendes, MD1, Rui Morais, MD1, Irene Gullo, MD, PhD2, Guilherme Macedo, MD, PhD, FACG1. P0699 - Underwater Endoscopic Mucosal Resection of Rectal Neuroendocrine Tumors – A Case Series of an Innovative Endoscopic Approach, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
