Sunday Poster Session
Category: General Endoscopy
P0704 - Unveiling the Unseen: Diagnosis of Appendicitis on Colonoscopy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Pujitha Vallivedu Chennakesavulu, MD, MBBS
Quinnipiac University Frank H. Netter MD School of Medicine / St. Vincent's Medical Center
Bridgeport, CT
Presenting Author(s)
Pujitha Vallivedu Chennakesavulu, MD, MBBS, Sushrut Ingawale, MD, MBBS, Monika Mishra, MD, MBBS
Quinnipiac University Frank H. Netter MD School of Medicine / St. Vincent's Medical Center, Bridgeport, CT
Introduction: Acute appendicitis is a well-established diagnosis with a definitive course. Colonoscopy has been increasingly prevalent due to recent increased awareness of colon cancer and screening discussion during the annual physical. Gastroscopy would never be a part of routine diagnostic algorithm as it is unlikely to have mortality benefit compared to risks. We discuss a case report of mucosal changes in colonoscopy that would prompt advanced diagnostics in an atypical presentation of appendicitis.
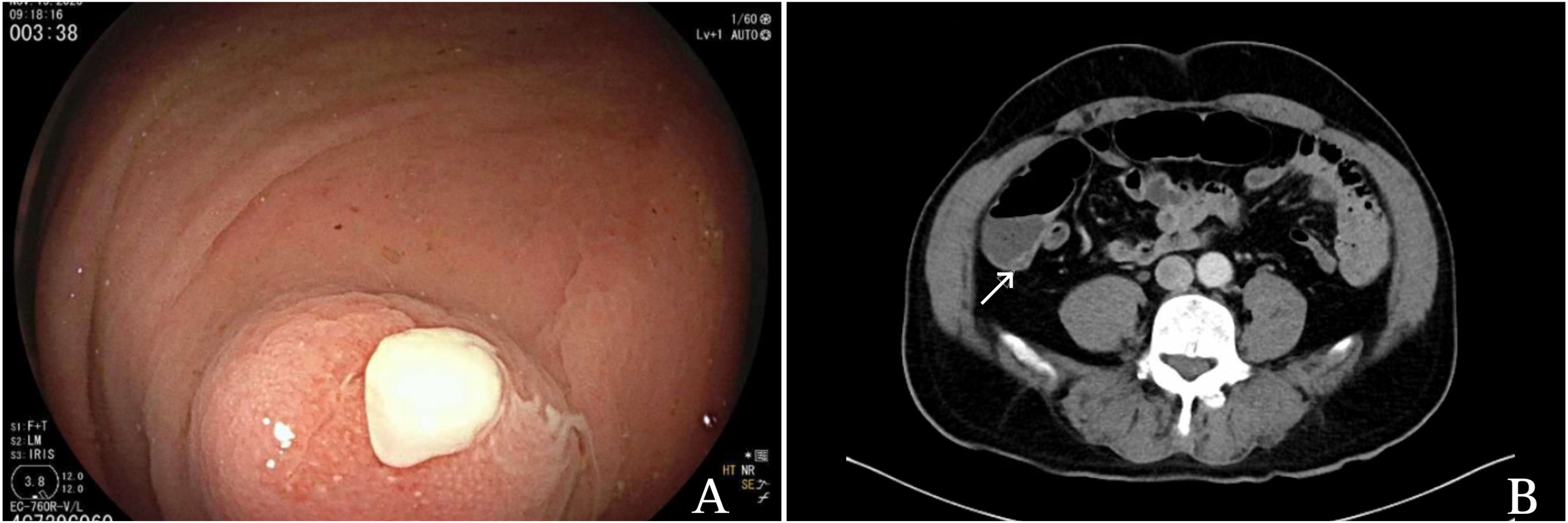
Case Description/Methods: A 79-year-old male with a past medical history of type 2 diabetes mellitus and resected colonic polyps presented to the primary care clinic for an annual physical examination. The patient denied any complaints of abdominal pain, nausea, vomiting, fever, chills, changes in bowel habits, or anorexia. The patient was referred to gastroenterology for a 10-year follow-up screening colonoscopy. During the colonoscopy, congested mucosa at the appendiceal orifice was noted, and purulence was observed at the orifice (Image A). A biopsy of inflamed mucosa was performed during the procedure. CT abdomen and pelvis revealed increased circumferential wall thickening at the appendiceal base with tapering towards the apex (Image B). The patient was asymptomatic and discharged home on amoxicillin-clavulanate. Elective laparoscopic appendectomy was performed on the next day with an insignificant postoperative course. Pathology of the biopsy specimen was consistent with acute appendicitis with fibrous obliteration of the tip.
Discussion: Acute appendicitis is a surgical emergency to prevent peritonitis from rupture of the inflamed appendix, ischemia, and abscess formation. The gold standard for the diagnosis is noncontrast CT abdomen and pelvis. The rate of negative appendectomy on pathology with suspicion on a CT scan is still persistently high, thus better diagnostic modalities are still in pursuit. There is limited published data on incidental diagnosis on colonoscopy; four published papers have presented the mucosal changes during colonoscopy. Endoscopic findings of suspected appendicitis include mucosal erythema, edema, abscess formation, and purulent discharge from the orifice. Immediate imaging with a CT abdomen can facilitate early diagnosis and intervention. Elective laparoscopic appendectomy remains the definitive treatment. Gastroenterologists should be aware of endoscopic findings of acute appendicitis and prompt to inculcate additional diagnostic modalities and surgical consultation.
Disclosures:
Pujitha Vallivedu Chennakesavulu, MD, MBBS, Sushrut Ingawale, MD, MBBS, Monika Mishra, MD, MBBS. P0704 - Unveiling the Unseen: Diagnosis of Appendicitis on Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Quinnipiac University Frank H. Netter MD School of Medicine / St. Vincent's Medical Center, Bridgeport, CT
Introduction: Acute appendicitis is a well-established diagnosis with a definitive course. Colonoscopy has been increasingly prevalent due to recent increased awareness of colon cancer and screening discussion during the annual physical. Gastroscopy would never be a part of routine diagnostic algorithm as it is unlikely to have mortality benefit compared to risks. We discuss a case report of mucosal changes in colonoscopy that would prompt advanced diagnostics in an atypical presentation of appendicitis.
Case Description/Methods: A 79-year-old male with a past medical history of type 2 diabetes mellitus and resected colonic polyps presented to the primary care clinic for an annual physical examination. The patient denied any complaints of abdominal pain, nausea, vomiting, fever, chills, changes in bowel habits, or anorexia. The patient was referred to gastroenterology for a 10-year follow-up screening colonoscopy. During the colonoscopy, congested mucosa at the appendiceal orifice was noted, and purulence was observed at the orifice (Image A). A biopsy of inflamed mucosa was performed during the procedure. CT abdomen and pelvis revealed increased circumferential wall thickening at the appendiceal base with tapering towards the apex (Image B). The patient was asymptomatic and discharged home on amoxicillin-clavulanate. Elective laparoscopic appendectomy was performed on the next day with an insignificant postoperative course. Pathology of the biopsy specimen was consistent with acute appendicitis with fibrous obliteration of the tip.
Discussion: Acute appendicitis is a surgical emergency to prevent peritonitis from rupture of the inflamed appendix, ischemia, and abscess formation. The gold standard for the diagnosis is noncontrast CT abdomen and pelvis. The rate of negative appendectomy on pathology with suspicion on a CT scan is still persistently high, thus better diagnostic modalities are still in pursuit. There is limited published data on incidental diagnosis on colonoscopy; four published papers have presented the mucosal changes during colonoscopy. Endoscopic findings of suspected appendicitis include mucosal erythema, edema, abscess formation, and purulent discharge from the orifice. Immediate imaging with a CT abdomen can facilitate early diagnosis and intervention. Elective laparoscopic appendectomy remains the definitive treatment. Gastroenterologists should be aware of endoscopic findings of acute appendicitis and prompt to inculcate additional diagnostic modalities and surgical consultation.
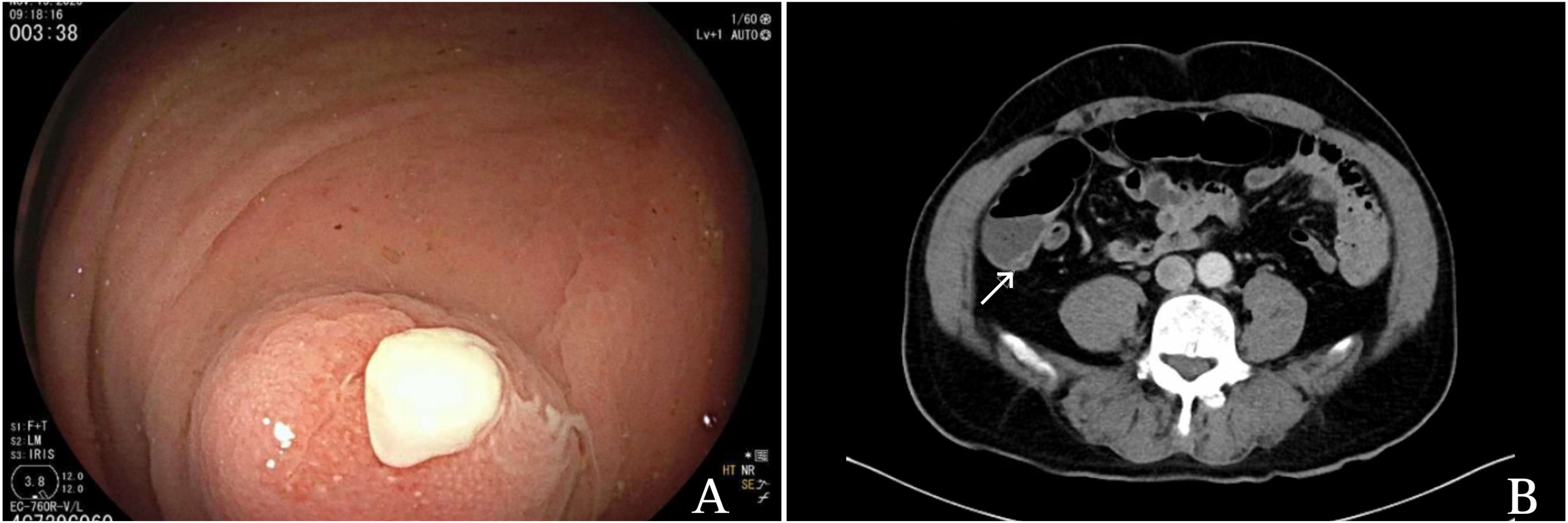
Figure: Image A: Purulent exudate with inflamed appendiceal orifice seen during colonoscopy; Image B: Inflamed appendix visualized in CT abdomen and pelvis
Disclosures:
Pujitha Vallivedu Chennakesavulu indicated no relevant financial relationships.
Sushrut Ingawale indicated no relevant financial relationships.
Monika Mishra indicated no relevant financial relationships.
Pujitha Vallivedu Chennakesavulu, MD, MBBS, Sushrut Ingawale, MD, MBBS, Monika Mishra, MD, MBBS. P0704 - Unveiling the Unseen: Diagnosis of Appendicitis on Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
