Sunday Poster Session
Category: General Endoscopy
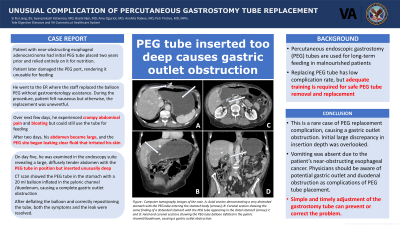
P0707 - Unusual Complication of Percutaneous Gastrostomy Tube Replacement
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- SL
Si Ru Liang, BS
Yale University School of Medicine
West Haven, CT
Presenting Author(s)
Si Ru Liang, BS1, Gyanprakash Ketwaroo, MD2, Basile Njei, MD3, Amy Ogurick, MD4, Anahita Rabiee, MD4, Petr Protiva, MD, MPH4
1Yale University School of Medicine, West Haven, CT; 2Yale Digestive Diseases and VA Connecticut Halthcare System, West Haven, CT; 3Yale University School of Medicine, New Haven, CT; 4Yale Digestive Diseases and VA Connecticut Healthcare System, West Haven, CT
Introduction: Percutaneous endoscopic gastrostomy (PEG) tubes are indicated for long-term feeding in patients with moderate-to-severe protein-calorie malnutrition. Initial endoscopic PEG placement is associated with low-risk adverse events and mortality. Once the gastrocutaneous fistula is formed and healed, replacing the PEG is straightforward and has a low complication rate. However, adequate training and expertise are required for safe PEG tube removal and replacement.
Case Description/Methods: A 63-year-old man with near-obstructing esophageal adenocarcinoma on palliative chemotherapy relied entirely on his PEG tube for nutrition. The initial PEG tube was placed endoscopically using the Ponsky pull method two years prior and was replaced once with a 20 French diameter balloon PEG due to clogging. The patient had no issues with the PEG tubes until he damaged the port, rendering it unusable for feeding.
He presented to the emergency room for PEG replacement. The emergency room staff replaced the balloon PEG without gastroenterology assistance. During the procedure, the patient felt nauseous but otherwise, the replacement was uneventful. He was cleared to use the tube immediately. Over the next few days, he experienced crampy abdominal pain and progressive bloating but could still use the tube for feeding. After two days, his abdomen became large, and the PEG site began leaking clear fluid that irritated his skin.
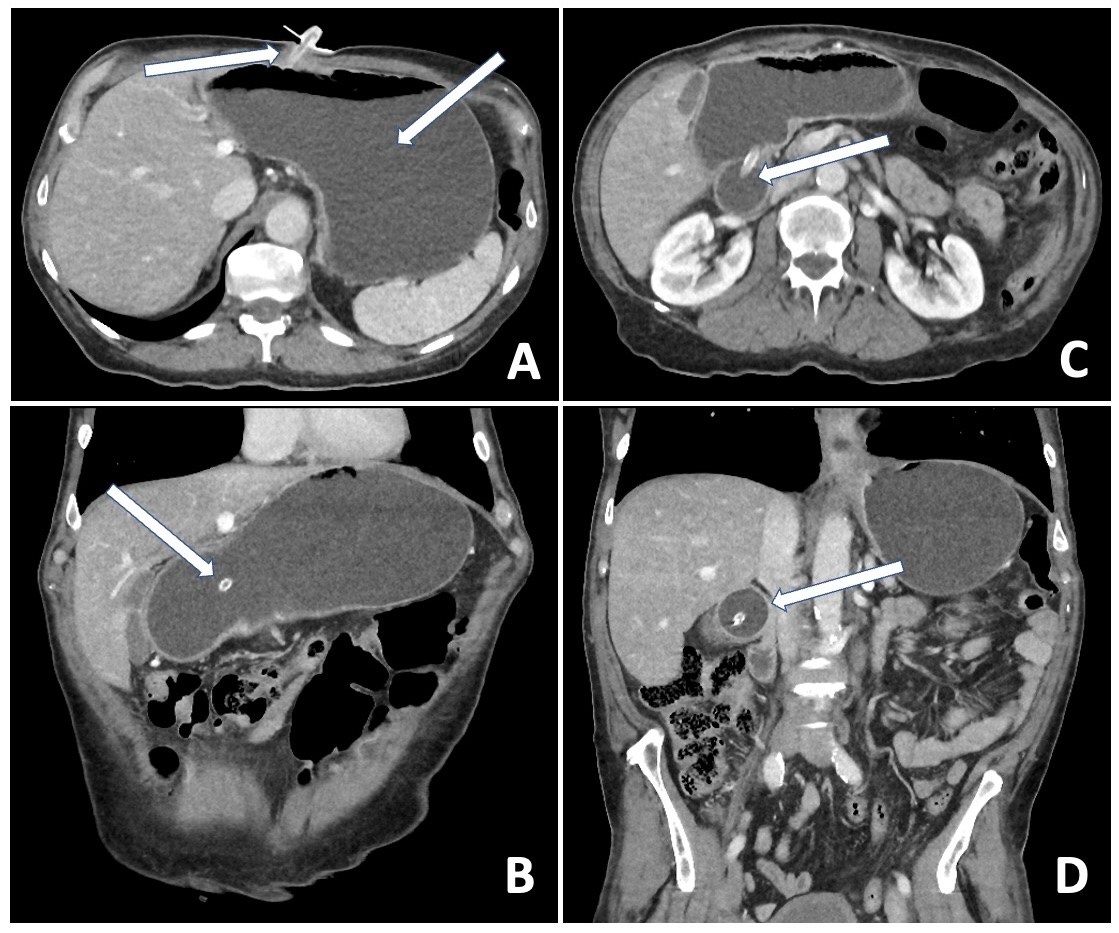
On day five, he presented to the endoscopy suite for urgent evaluation revealing a large, diffusely tender abdomen with the PEG tube in position but inserted unusually deep beyond the typical several centimeters. An emergency CT scan showed the PEG tube in the stomach with a 20 ml balloon inflated in the pyloric channel/duodenum, causing a complete gastric outlet obstruction (Figure). The service gastroenterologist deflated the PEG balloon, repositioned the tube correctly, resolving both the symptoms and the leak. The patient was admitted for rehydration and observation and discharged the next day.
Discussion: This is a rare case of PEG replacement complication, causing a gastric outlet obstruction. Initial large discrepancy in insertion depth was overlooked. Vomiting was absent due to the patient’s near-obstructing esophageal cancer. Physicians should be aware of potential gastric outlet and duodenal obstruction as complications of PEG tube placement. Simple and timely adjustment of the gastrostomy tube can prevent or correct the problem.
Disclosures:
Si Ru Liang, BS1, Gyanprakash Ketwaroo, MD2, Basile Njei, MD3, Amy Ogurick, MD4, Anahita Rabiee, MD4, Petr Protiva, MD, MPH4. P0707 - Unusual Complication of Percutaneous Gastrostomy Tube Replacement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Yale University School of Medicine, West Haven, CT; 2Yale Digestive Diseases and VA Connecticut Halthcare System, West Haven, CT; 3Yale University School of Medicine, New Haven, CT; 4Yale Digestive Diseases and VA Connecticut Healthcare System, West Haven, CT
Introduction: Percutaneous endoscopic gastrostomy (PEG) tubes are indicated for long-term feeding in patients with moderate-to-severe protein-calorie malnutrition. Initial endoscopic PEG placement is associated with low-risk adverse events and mortality. Once the gastrocutaneous fistula is formed and healed, replacing the PEG is straightforward and has a low complication rate. However, adequate training and expertise are required for safe PEG tube removal and replacement.
Case Description/Methods: A 63-year-old man with near-obstructing esophageal adenocarcinoma on palliative chemotherapy relied entirely on his PEG tube for nutrition. The initial PEG tube was placed endoscopically using the Ponsky pull method two years prior and was replaced once with a 20 French diameter balloon PEG due to clogging. The patient had no issues with the PEG tubes until he damaged the port, rendering it unusable for feeding.
He presented to the emergency room for PEG replacement. The emergency room staff replaced the balloon PEG without gastroenterology assistance. During the procedure, the patient felt nauseous but otherwise, the replacement was uneventful. He was cleared to use the tube immediately. Over the next few days, he experienced crampy abdominal pain and progressive bloating but could still use the tube for feeding. After two days, his abdomen became large, and the PEG site began leaking clear fluid that irritated his skin.
On day five, he presented to the endoscopy suite for urgent evaluation revealing a large, diffusely tender abdomen with the PEG tube in position but inserted unusually deep beyond the typical several centimeters. An emergency CT scan showed the PEG tube in the stomach with a 20 ml balloon inflated in the pyloric channel/duodenum, causing a complete gastric outlet obstruction (Figure). The service gastroenterologist deflated the PEG balloon, repositioned the tube correctly, resolving both the symptoms and the leak. The patient was admitted for rehydration and observation and discharged the next day.
Discussion: This is a rare case of PEG replacement complication, causing a gastric outlet obstruction. Initial large discrepancy in insertion depth was overlooked. Vomiting was absent due to the patient’s near-obstructing esophageal cancer. Physicians should be aware of potential gastric outlet and duodenal obstruction as complications of PEG tube placement. Simple and timely adjustment of the gastrostomy tube can prevent or correct the problem.
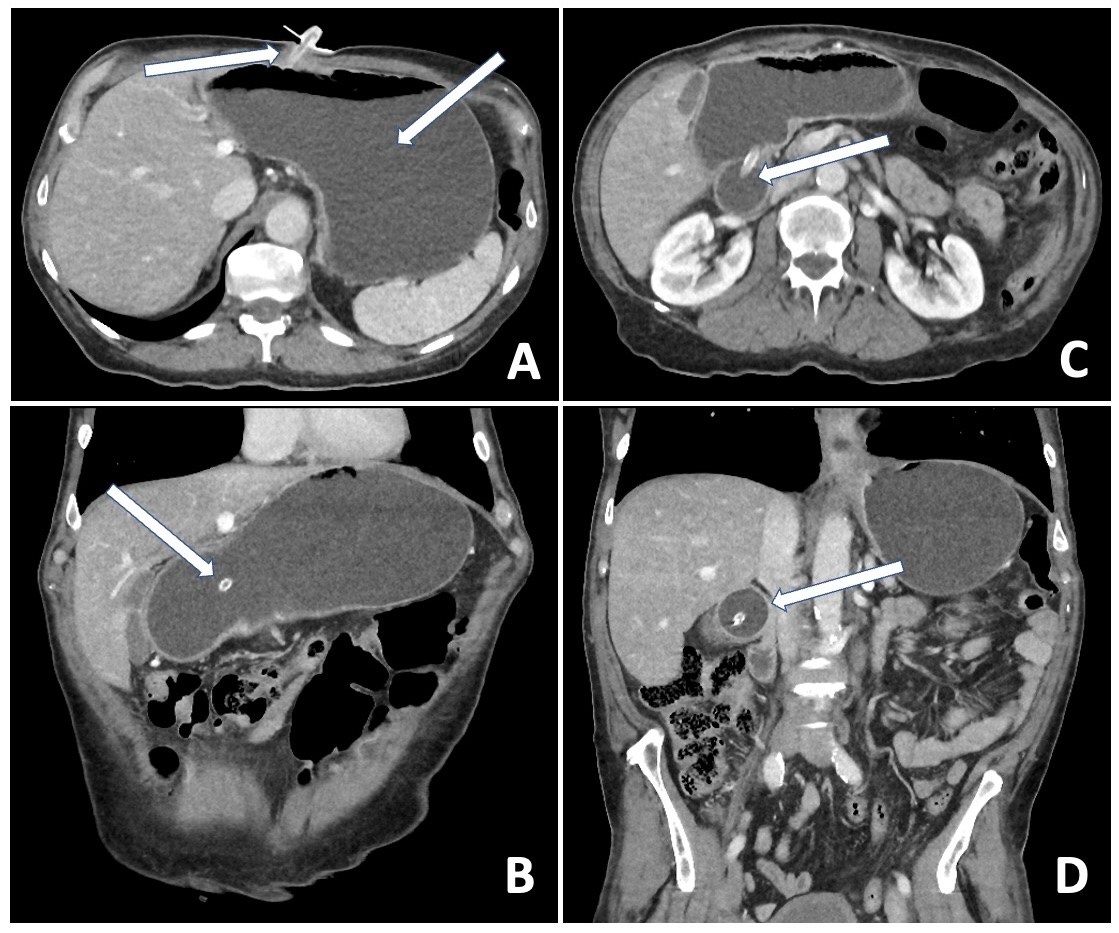
Figure: Figure: Computer tomography images of the case. A: Axial section demonstrating a very distended stomach with the PEG tube entering the stomach body (arrows); B: Coronal section showing the same finding of a distended stomach with the PEG tube appearing in the distal stomach (arrow); C and D: Axial and coronal sections showing the PEG tube balloon inflated in the pyloric channel/duodenum, causing a gastric outlet obstruction.
Disclosures:
Si Ru Liang indicated no relevant financial relationships.
Gyanprakash Ketwaroo indicated no relevant financial relationships.
Basile Njei indicated no relevant financial relationships.
Amy Ogurick indicated no relevant financial relationships.
Anahita Rabiee indicated no relevant financial relationships.
Petr Protiva indicated no relevant financial relationships.
Si Ru Liang, BS1, Gyanprakash Ketwaroo, MD2, Basile Njei, MD3, Amy Ogurick, MD4, Anahita Rabiee, MD4, Petr Protiva, MD, MPH4. P0707 - Unusual Complication of Percutaneous Gastrostomy Tube Replacement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
