Sunday Poster Session
Category: GI Bleeding
P0739 - Analysis of Gastrointestinal Bleed in Patients Undergoing ECMO Based on Approach: An Inpatient Database Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ayusha Poudel, MD
Cook County Health
Chicago, IL
Presenting Author(s)
Ayusha Poudel, MD1, Anurag Adhikari, MD2, Sajana Poudel, MD3, Aayush Poudel, BSc4
1Cook County Health, Chicago, IL; 2NYC Health + Hospitals/Jacobi, New York, NY; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 4University of Rochester, Charlotte, NC
Introduction: Our study aims to analyze the influence of gastrointestinal (GI) bleeding in patients undergoing extracorporeal membrane oxygenation (ECMO) using real-world data from the National Inpatient Survey (2016-2020). GI bleeding is a common complication during ECMO, linked to increased mortality and healthcare costs. Despite limited literature on this topic, our research seeks to investigate outcomes, predisposing factors, and associated complications in ECMO patients with GI bleed, comparing central and peripheral approaches.
This study aims to provide valuable insights for optimizing management and improving outcomes in this patient population.
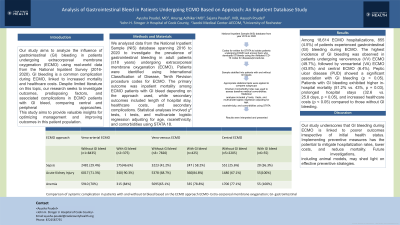
Methods: We analyzed data from the National Inpatient Sample (NIS) database spanning 2016 to 2020 to investigate the prevalence of gastrointestinal bleeding in adult patients (≥18 years) undergoing extracorporeal membrane oxygenation (ECMO). Patients were identified using International Classification of Disease, Tenth Revision procedure codes for ECMO. The primary outcome was inpatient mortality among ECMO patients with GI bleed depending on the approach used, while secondary outcomes included length of hospital stay, healthcare costs, and secondary complications. Statistical analyses involved χ² tests, t tests, and multivariate logistic regression adjusting for age, race/ethnicity, and comorbidities using STATA 18.
Results: Among 18,614 ECMO hospitalizations, 855 (4.5%) of patients experienced gastrointestinal (GI) bleeding during ECMO. The highest incidence of GI bleeding was observed in patients undergoing venovenous (VV) ECMO (49.7%), followed by venoarterial (VA) ECMO (43.8%) and central ECMO (6.4%). Peptic ulcer disease (PUD) showed a significant association with GI bleeding (p < 0.05). Patients with GI bleeding exhibited higher in-hospital mortality (51.2% vs. 43%, p = 0.03), prolonged hospital stays (32.6 vs.
25.8 days, p < 0.05), and increased healthcare costs (p < 0.05) compared to those without GI bleeding.
Discussion: Our study underscores that GI bleeding during ECMO is linked to poorer outcomes irrespective of initial health status. Implementing preventive measures has the potential to mitigate hospitalization rates, lower costs, and reduce mortality. Future investigations,
including animal models, may shed light on effective preventive strategies.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ayusha Poudel, MD1, Anurag Adhikari, MD2, Sajana Poudel, MD3, Aayush Poudel, BSc4. P0739 - Analysis of Gastrointestinal Bleed in Patients Undergoing ECMO Based on Approach: An Inpatient Database Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cook County Health, Chicago, IL; 2NYC Health + Hospitals/Jacobi, New York, NY; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 4University of Rochester, Charlotte, NC
Introduction: Our study aims to analyze the influence of gastrointestinal (GI) bleeding in patients undergoing extracorporeal membrane oxygenation (ECMO) using real-world data from the National Inpatient Survey (2016-2020). GI bleeding is a common complication during ECMO, linked to increased mortality and healthcare costs. Despite limited literature on this topic, our research seeks to investigate outcomes, predisposing factors, and associated complications in ECMO patients with GI bleed, comparing central and peripheral approaches.
This study aims to provide valuable insights for optimizing management and improving outcomes in this patient population.
Methods: We analyzed data from the National Inpatient Sample (NIS) database spanning 2016 to 2020 to investigate the prevalence of gastrointestinal bleeding in adult patients (≥18 years) undergoing extracorporeal membrane oxygenation (ECMO). Patients were identified using International Classification of Disease, Tenth Revision procedure codes for ECMO. The primary outcome was inpatient mortality among ECMO patients with GI bleed depending on the approach used, while secondary outcomes included length of hospital stay, healthcare costs, and secondary complications. Statistical analyses involved χ² tests, t tests, and multivariate logistic regression adjusting for age, race/ethnicity, and comorbidities using STATA 18.
Results: Among 18,614 ECMO hospitalizations, 855 (4.5%) of patients experienced gastrointestinal (GI) bleeding during ECMO. The highest incidence of GI bleeding was observed in patients undergoing venovenous (VV) ECMO (49.7%), followed by venoarterial (VA) ECMO (43.8%) and central ECMO (6.4%). Peptic ulcer disease (PUD) showed a significant association with GI bleeding (p < 0.05). Patients with GI bleeding exhibited higher in-hospital mortality (51.2% vs. 43%, p = 0.03), prolonged hospital stays (32.6 vs.
25.8 days, p < 0.05), and increased healthcare costs (p < 0.05) compared to those without GI bleeding.
Discussion: Our study underscores that GI bleeding during ECMO is linked to poorer outcomes irrespective of initial health status. Implementing preventive measures has the potential to mitigate hospitalization rates, lower costs, and reduce mortality. Future investigations,
including animal models, may shed light on effective preventive strategies.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ayusha Poudel indicated no relevant financial relationships.
Anurag Adhikari indicated no relevant financial relationships.
Sajana Poudel indicated no relevant financial relationships.
Aayush Poudel indicated no relevant financial relationships.
Ayusha Poudel, MD1, Anurag Adhikari, MD2, Sajana Poudel, MD3, Aayush Poudel, BSc4. P0739 - Analysis of Gastrointestinal Bleed in Patients Undergoing ECMO Based on Approach: An Inpatient Database Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
