Sunday Poster Session
Category: GI Bleeding
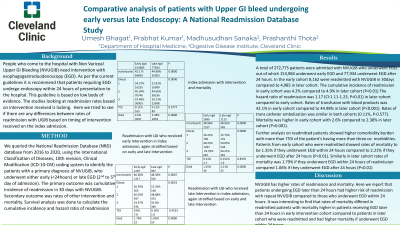
P0740 - Comparative Analysis of Patients With Upper GI Bleed Undergoing Early versus Late Endoscopy: A National Readmission Database Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- UB
Umesh Bhagat, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Umesh Bhagat, MD1, Ankit Agrawal, MD1, Prabhat NA. Kumar, MD2, Shalini Tripathi, MD1, Mounir Ibrahim, MD1, Archana Kahrel, MD1, Anshu Priya, MD3, Prashanthi N. Thota, MD1, Madhusudhan R. Sanaka, MD1
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, FL; 3Charleston Area Medical Center, Charleston, WV
Introduction: Patients with Non Variceal Upper GI Bleed(GIB) need intervention with esophagogastroduodenoscopy (EGD).Per the current guidelines it is recommend that patients undergo EGD within 24hours. This guideline is based on low quality of evidence. The studies looking at readmission rates based on intervention received is lacking. Here we tried to see if there are any differences between rates of readmission with GIB based on timing of intervention in the index admission
Methods: We queried the NRD database from 2016 to 2020, using ICD-10-CM coding system to identify the patients with a primary diagnosis of GIB, who underwent either early (< 24hours) or late EGD ( >24hours). The primary outcome was cumulative incidence (CI) of readmission in 30 days with NVUGIB. Secondary outcome was rates of other intervention and mortality. Survival analysis was done to calculate the CI and HR of readmission
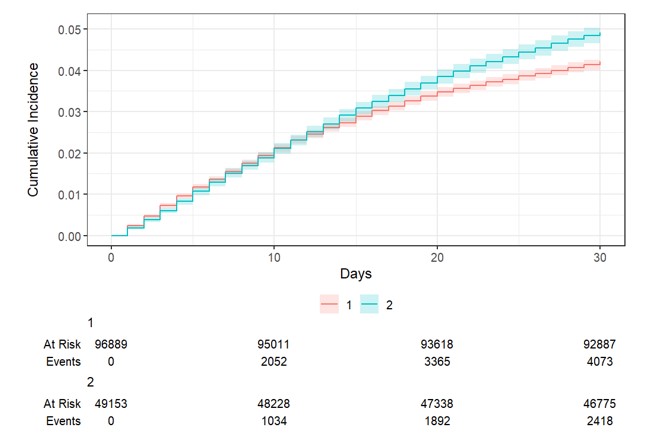
Results: Total of 272,775 patients were admitted with GIB who underwent EGD, out of which 153,984 underwent early (< 24 hours) EGD and 77,934 underwent EGD late ( >24 hours). In the early cohort 8,162 were readmitted with GIB in 30days compared to 4,985 in late cohort. The CI of readmission in early cohort was 4.2% compared to 4.9% in late cohort (P< 0.01) The HR of readmission was 1.17 (CI:1.11-1.23,P< 0.01) in late cohort compared to early cohort. Rates of transfusion with blood products was 42.1% in early cohort compared to 44.98% in late cohort (P< 0.001). Rates of embolization was similar in both cohorts (0.11%, P-0.577). Mortality was higher in early cohort with 2.6% compared to 2.38% in late cohort (P< 0.001).Analysis on readmitted patients showed higher comorbidity burden with >75% with >3 comorbidities. Patients from early cohort who were readmitted showed rates of mortality to be 1.35% if they underwent EGD early compared to 2.21% if they underwent EGD late (P< 0.01). Similarly in late cohort rates of mortality was 1.79% if they underwent EGD < 24 hours of readmission compared 1.06% if they underwent EGD late(P< 0.01)
Discussion: GIB has higher rates of readmission and mortality. Here we report that patients undergoing EGD later had higher risk of readmission with repeat GIB compared to those who underwent EGD late. It was interesting to find that rates of mortality differed in readmitted patients with mortality higher in patients receiving EGD >24hours in early intervention cohort compared to patients in later cohort who were readmitted and had higher mortality if they underwent EGD < 24hours
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Umesh Bhagat, MD1, Ankit Agrawal, MD1, Prabhat NA. Kumar, MD2, Shalini Tripathi, MD1, Mounir Ibrahim, MD1, Archana Kahrel, MD1, Anshu Priya, MD3, Prashanthi N. Thota, MD1, Madhusudhan R. Sanaka, MD1. P0740 - Comparative Analysis of Patients With Upper GI Bleed Undergoing Early versus Late Endoscopy: A National Readmission Database Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, FL; 3Charleston Area Medical Center, Charleston, WV
Introduction: Patients with Non Variceal Upper GI Bleed(GIB) need intervention with esophagogastroduodenoscopy (EGD).Per the current guidelines it is recommend that patients undergo EGD within 24hours. This guideline is based on low quality of evidence. The studies looking at readmission rates based on intervention received is lacking. Here we tried to see if there are any differences between rates of readmission with GIB based on timing of intervention in the index admission
Methods: We queried the NRD database from 2016 to 2020, using ICD-10-CM coding system to identify the patients with a primary diagnosis of GIB, who underwent either early (< 24hours) or late EGD ( >24hours). The primary outcome was cumulative incidence (CI) of readmission in 30 days with NVUGIB. Secondary outcome was rates of other intervention and mortality. Survival analysis was done to calculate the CI and HR of readmission
Results: Total of 272,775 patients were admitted with GIB who underwent EGD, out of which 153,984 underwent early (< 24 hours) EGD and 77,934 underwent EGD late ( >24 hours). In the early cohort 8,162 were readmitted with GIB in 30days compared to 4,985 in late cohort. The CI of readmission in early cohort was 4.2% compared to 4.9% in late cohort (P< 0.01) The HR of readmission was 1.17 (CI:1.11-1.23,P< 0.01) in late cohort compared to early cohort. Rates of transfusion with blood products was 42.1% in early cohort compared to 44.98% in late cohort (P< 0.001). Rates of embolization was similar in both cohorts (0.11%, P-0.577). Mortality was higher in early cohort with 2.6% compared to 2.38% in late cohort (P< 0.001).Analysis on readmitted patients showed higher comorbidity burden with >75% with >3 comorbidities. Patients from early cohort who were readmitted showed rates of mortality to be 1.35% if they underwent EGD early compared to 2.21% if they underwent EGD late (P< 0.01). Similarly in late cohort rates of mortality was 1.79% if they underwent EGD < 24 hours of readmission compared 1.06% if they underwent EGD late(P< 0.01)
Discussion: GIB has higher rates of readmission and mortality. Here we report that patients undergoing EGD later had higher risk of readmission with repeat GIB compared to those who underwent EGD late. It was interesting to find that rates of mortality differed in readmitted patients with mortality higher in patients receiving EGD >24hours in early intervention cohort compared to patients in later cohort who were readmitted and had higher mortality if they underwent EGD < 24hours
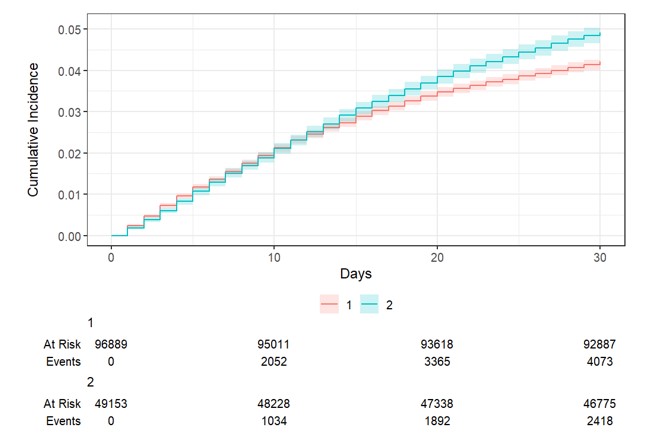
Figure: Image showing the CI of readmission, 1-Early cohort, 2-late cohort
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Umesh Bhagat indicated no relevant financial relationships.
Ankit Agrawal indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Shalini Tripathi indicated no relevant financial relationships.
Mounir Ibrahim indicated no relevant financial relationships.
Archana Kahrel indicated no relevant financial relationships.
Anshu Priya indicated no relevant financial relationships.
Prashanthi Thota indicated no relevant financial relationships.
Madhusudhan R. Sanaka indicated no relevant financial relationships.
Umesh Bhagat, MD1, Ankit Agrawal, MD1, Prabhat NA. Kumar, MD2, Shalini Tripathi, MD1, Mounir Ibrahim, MD1, Archana Kahrel, MD1, Anshu Priya, MD3, Prashanthi N. Thota, MD1, Madhusudhan R. Sanaka, MD1. P0740 - Comparative Analysis of Patients With Upper GI Bleed Undergoing Early versus Late Endoscopy: A National Readmission Database Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
