Sunday Poster Session
Category: GI Bleeding
P0747 - Bacterial Infections in Variceal Hemorrhage: A National Study of Clinical Impact
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Ali Jaan, MD
Rochester General Hospital
Rochester, NY
Presenting Author(s)
Ali Jaan, MD1, Adeena Maryyum, MBBS2, Ammad Javaid. Chaudhary, MD3, Nosheen Hafeez, MD4, Ashish Dhawan, MBBS5, Laraib Fatima. Sheikh, 6, Sushil Ahlawat, MD, MS, MBBS7
1Rochester General Hospital, Rochester, NY; 2Ayub Medical College, Abbottabad, North-West Frontier, Pakistan; 3Henry Ford Health, Detroit, MI; 4Baptist Health-University of Arkansas for Medical Sciences, North Little Rock, AR; 5Gian Sagar Medical College and Hospital, Chandigarh, Chandigarh, India; 6Lahore Medical and Dental College, Rochester, NY; 7SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Variceal upper gastrointestinal bleeding (VUGIB) presents a critical challenge in clinical settings, often complicated by the development of concurrent infections. This study seeks to determine the incidence and clinical implications of VUGIB hospitalizations complicated with infections.
Methods: Using the National Readmission Database 2019, we employed the International Classification of Diseases, 10th revision, Clinical Modifications (ICD-10-CM) codes to identify adult patients (age >18 years) admitted with VUGIB. We further stratified VUGIB hospitalizations based on the presence of a concurrent same-admission infection (i.e., pneumonia, spontaneous bacterial peritonitis (SBP), urinary tract infection (UTI), or bacteremia). Utilizing a multivariate regression model, we compared the impact of secondary infection on the outcomes and procedural performance of VUGIB patients. STATA 14.2 was utilized for statistical analysis.
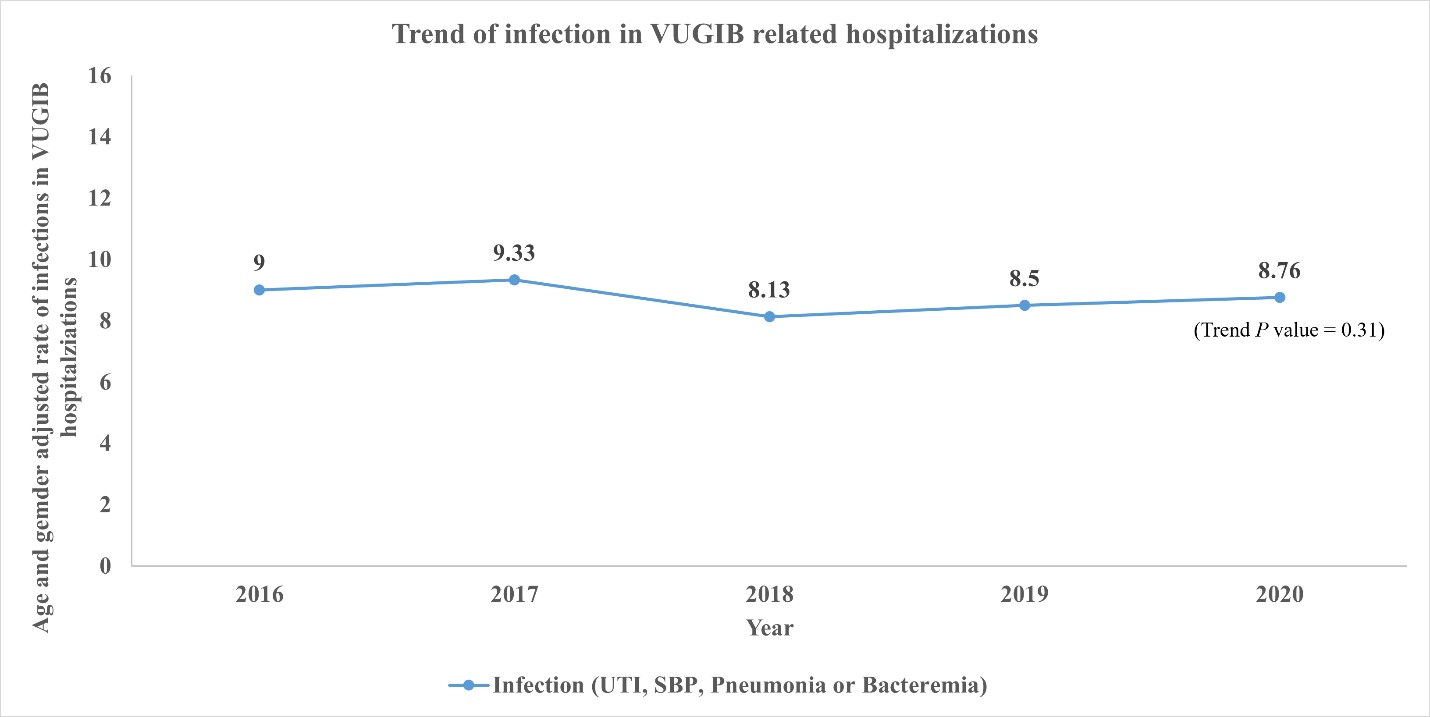
Results: Among the 9,565 VUGIB patients, 750 (8.5%) developed infections (Table 1). Of these, 43.2 % had a urinary tract infection (UTI), 35.89% had bacterial pneumonia, while bacteremia was present in 7.70%. Adjusted analyses revealed that VUGIB patients who developed concurrent infections exhibited significantly higher odds of mortality (adjusted odds ratio [aOR]: 2.36, P < 0.001), alongside an increased likelihood of complications such as hemorrhagic shock (aOR: 1.84), hepatorenal syndrome (aOR: 3.32), need for vasopressors ( aOR: 2.13) and mechanical ventilation (aOR: 3.47) (Table 1). Moreover, those who developed infections had higher odds of requiring repeat esophagogastroduodenoscopy (EGD) (aOR: 1.52) and transjugular intrahepatic portosystemic shunt (TIPS) (aOR: 1.54). Finally, resource utilization, as estimated by total parenteral nutrition requirement, rehabilitation discharge, length of hospital stay, and hospitalization charges, was substantially higher in patients who developed infection (P< 0.001). Longitudinal analysis over 2016-2020 did not show a statistically significant change in rates of infection (Figure 1).
Discussion: Our study revealed that infections among VUGIB patients are associated with markedly worse clinical outcomes, including higher mortality, hemorrhagic shock, rebleeding requiring repeat EGD and need for TIPS. These findings underscore the need for vigilant infection prevention and management strategies to improve patient prognosis and alleviate the burden on the healthcare system.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ali Jaan, MD1, Adeena Maryyum, MBBS2, Ammad Javaid. Chaudhary, MD3, Nosheen Hafeez, MD4, Ashish Dhawan, MBBS5, Laraib Fatima. Sheikh, 6, Sushil Ahlawat, MD, MS, MBBS7. P0747 - Bacterial Infections in Variceal Hemorrhage: A National Study of Clinical Impact, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Rochester General Hospital, Rochester, NY; 2Ayub Medical College, Abbottabad, North-West Frontier, Pakistan; 3Henry Ford Health, Detroit, MI; 4Baptist Health-University of Arkansas for Medical Sciences, North Little Rock, AR; 5Gian Sagar Medical College and Hospital, Chandigarh, Chandigarh, India; 6Lahore Medical and Dental College, Rochester, NY; 7SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Variceal upper gastrointestinal bleeding (VUGIB) presents a critical challenge in clinical settings, often complicated by the development of concurrent infections. This study seeks to determine the incidence and clinical implications of VUGIB hospitalizations complicated with infections.
Methods: Using the National Readmission Database 2019, we employed the International Classification of Diseases, 10th revision, Clinical Modifications (ICD-10-CM) codes to identify adult patients (age >18 years) admitted with VUGIB. We further stratified VUGIB hospitalizations based on the presence of a concurrent same-admission infection (i.e., pneumonia, spontaneous bacterial peritonitis (SBP), urinary tract infection (UTI), or bacteremia). Utilizing a multivariate regression model, we compared the impact of secondary infection on the outcomes and procedural performance of VUGIB patients. STATA 14.2 was utilized for statistical analysis.
Results: Among the 9,565 VUGIB patients, 750 (8.5%) developed infections (Table 1). Of these, 43.2 % had a urinary tract infection (UTI), 35.89% had bacterial pneumonia, while bacteremia was present in 7.70%. Adjusted analyses revealed that VUGIB patients who developed concurrent infections exhibited significantly higher odds of mortality (adjusted odds ratio [aOR]: 2.36, P < 0.001), alongside an increased likelihood of complications such as hemorrhagic shock (aOR: 1.84), hepatorenal syndrome (aOR: 3.32), need for vasopressors ( aOR: 2.13) and mechanical ventilation (aOR: 3.47) (Table 1). Moreover, those who developed infections had higher odds of requiring repeat esophagogastroduodenoscopy (EGD) (aOR: 1.52) and transjugular intrahepatic portosystemic shunt (TIPS) (aOR: 1.54). Finally, resource utilization, as estimated by total parenteral nutrition requirement, rehabilitation discharge, length of hospital stay, and hospitalization charges, was substantially higher in patients who developed infection (P< 0.001). Longitudinal analysis over 2016-2020 did not show a statistically significant change in rates of infection (Figure 1).
Discussion: Our study revealed that infections among VUGIB patients are associated with markedly worse clinical outcomes, including higher mortality, hemorrhagic shock, rebleeding requiring repeat EGD and need for TIPS. These findings underscore the need for vigilant infection prevention and management strategies to improve patient prognosis and alleviate the burden on the healthcare system.
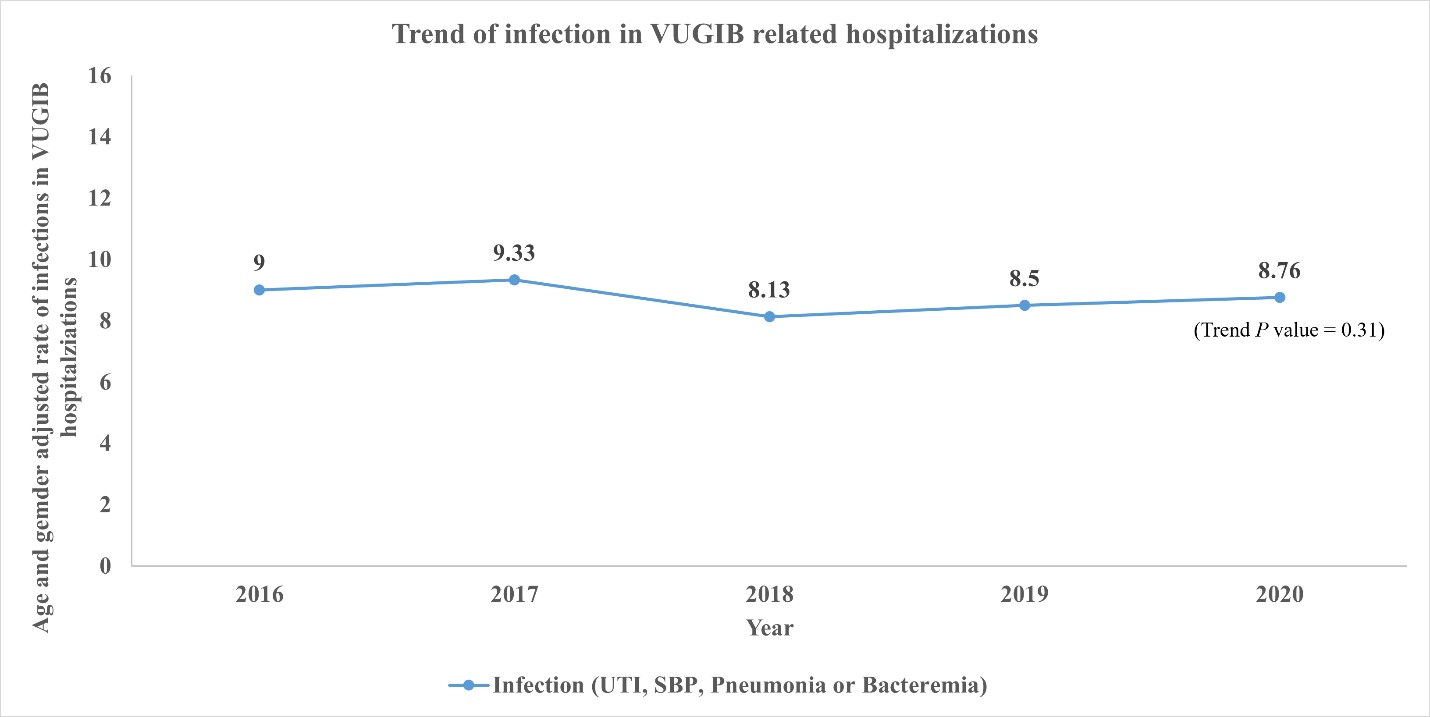
Figure: Figure 1: Longitudinal analysis of infection in variceal upper gastrointestinal bleeding hospitalizations.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ali Jaan indicated no relevant financial relationships.
Adeena Maryyum indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Nosheen Hafeez indicated no relevant financial relationships.
Ashish Dhawan indicated no relevant financial relationships.
Laraib Sheikh indicated no relevant financial relationships.
Sushil Ahlawat indicated no relevant financial relationships.
Ali Jaan, MD1, Adeena Maryyum, MBBS2, Ammad Javaid. Chaudhary, MD3, Nosheen Hafeez, MD4, Ashish Dhawan, MBBS5, Laraib Fatima. Sheikh, 6, Sushil Ahlawat, MD, MS, MBBS7. P0747 - Bacterial Infections in Variceal Hemorrhage: A National Study of Clinical Impact, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
