Sunday Poster Session
Category: GI Bleeding
P0770 - Post-Polypectomy Coagulation Syndrome Presenting as Hematochezia and Syncopal Episodes: A Complication of Electrocoagulation
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Kojo-Frimpong B. Awuah, MD
Allegheny General Hospital
Pittsburgh, PA
Presenting Author(s)
Kojo-Frimpong B. Awuah, MD, Tyrell Daniel, MD, Alexandra M. Johnston, DO
Allegheny General Hospital, Pittsburgh, PA
Introduction: A rare complication of polypectomy is post-polypectomy coagulation syndrome (PPCS), which may cause fever, abdominal pain, and bleeding. While useful for the removal of larger polyps, electrocoagulation can lead to complications. We report a case of PPCS presenting as hematochezia and syncope post-electrocoagulation polypectomy.
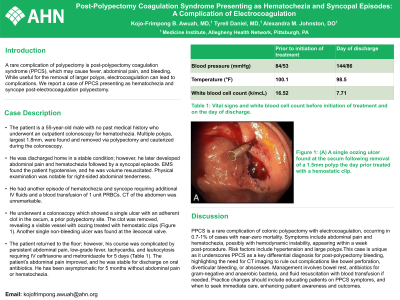
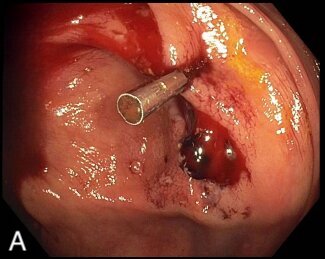
Case Description/Methods: The patient is a 55 year old male with no past medical history who underwent an outpatient colonoscopy for hematochezia. Multiple polyps, largest 1.8mm, were found, and removed via polypectomy and cauterized during the colonoscopy. He was discharged home in a stable condition, however, he later developed abdominal pain, and hematochezia followed by a syncopal episode. EMS found the patient hypotensive, and he was volume resuscitated. Physical examination was notable for right-sided abdominal tenderness. He had another episode of hematochezia and syncope requiring additional IV fluids and a blood transfusion of 1 unit PRBCs. CT of the abdomen was unremarkable. He underwent a colonoscopy which showed a single ulcer with an adherent clot in the cecum, a prior polypectomy site. The clot was removed revealing a visible vessel with oozing treated with hemostatic clips (Figure 1). Another single non-bleeding ulcer was found at the ileocecal valve. The patient returned to the floor; however, his course was complicated by persistent abdominal pain, low-grade fever, tachycardia, and leukocytosis requiring IV ceftriaxone and metronidazole for 5 days (Table 1). The patient’s abdominal pain improved and he was stable for discharge on oral antibiotics. He has been asymptomatic for 5 months without abdominal pain or hematochezia.
Discussion: PPCS is a rare complication of colonic polypectomy with electrocoagulation, occurring in 0.7-1% of cases with near-zero mortality. Symptoms include abdominal pain and hematochezia, possibly with hemodynamic instability, appearing within a week post-procedure. Risk factors include hypertension and large polyps.This case is unique as it underscores PPCS as a key differential diagnosis for post-polypectomy bleeding, highlighting the need for CT imaging to rule out complications like bowel perforation, diverticular bleeding, or abscesses. Management involves bowel rest, antibiotics for gram-negative and anaerobic bacteria, and fluid resuscitation with blood transfusion if needed. Practice changes should include educating patients on PPCS symptoms, and when to seek immediate care, enhancing patient awareness and outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kojo-Frimpong B. Awuah, MD, Tyrell Daniel, MD, Alexandra M. Johnston, DO. P0770 - Post-Polypectomy Coagulation Syndrome Presenting as Hematochezia and Syncopal Episodes: A Complication of Electrocoagulation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Allegheny General Hospital, Pittsburgh, PA
Introduction: A rare complication of polypectomy is post-polypectomy coagulation syndrome (PPCS), which may cause fever, abdominal pain, and bleeding. While useful for the removal of larger polyps, electrocoagulation can lead to complications. We report a case of PPCS presenting as hematochezia and syncope post-electrocoagulation polypectomy.
Case Description/Methods: The patient is a 55 year old male with no past medical history who underwent an outpatient colonoscopy for hematochezia. Multiple polyps, largest 1.8mm, were found, and removed via polypectomy and cauterized during the colonoscopy. He was discharged home in a stable condition, however, he later developed abdominal pain, and hematochezia followed by a syncopal episode. EMS found the patient hypotensive, and he was volume resuscitated. Physical examination was notable for right-sided abdominal tenderness. He had another episode of hematochezia and syncope requiring additional IV fluids and a blood transfusion of 1 unit PRBCs. CT of the abdomen was unremarkable. He underwent a colonoscopy which showed a single ulcer with an adherent clot in the cecum, a prior polypectomy site. The clot was removed revealing a visible vessel with oozing treated with hemostatic clips (Figure 1). Another single non-bleeding ulcer was found at the ileocecal valve. The patient returned to the floor; however, his course was complicated by persistent abdominal pain, low-grade fever, tachycardia, and leukocytosis requiring IV ceftriaxone and metronidazole for 5 days (Table 1). The patient’s abdominal pain improved and he was stable for discharge on oral antibiotics. He has been asymptomatic for 5 months without abdominal pain or hematochezia.
Discussion: PPCS is a rare complication of colonic polypectomy with electrocoagulation, occurring in 0.7-1% of cases with near-zero mortality. Symptoms include abdominal pain and hematochezia, possibly with hemodynamic instability, appearing within a week post-procedure. Risk factors include hypertension and large polyps.This case is unique as it underscores PPCS as a key differential diagnosis for post-polypectomy bleeding, highlighting the need for CT imaging to rule out complications like bowel perforation, diverticular bleeding, or abscesses. Management involves bowel rest, antibiotics for gram-negative and anaerobic bacteria, and fluid resuscitation with blood transfusion if needed. Practice changes should include educating patients on PPCS symptoms, and when to seek immediate care, enhancing patient awareness and outcomes.
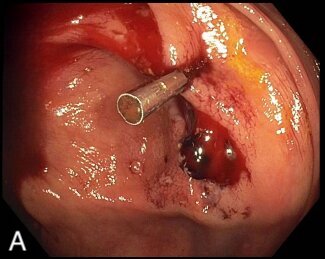
Figure: Figure 1: (A) A single oozing ulcer found at the cecum following removal of a 1.5mm polyp the day prior treated with a hemostatic clip.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kojo-Frimpong Awuah indicated no relevant financial relationships.
Tyrell Daniel indicated no relevant financial relationships.
Alexandra Johnston indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah, MD, Tyrell Daniel, MD, Alexandra M. Johnston, DO. P0770 - Post-Polypectomy Coagulation Syndrome Presenting as Hematochezia and Syncopal Episodes: A Complication of Electrocoagulation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
