Sunday Poster Session
Category: GI Bleeding
P0783 - An Interesting Case of a Descending Colonic Varix Unresponsive to Transjugular Intrahepatic Portosystemic Shunt Placement
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- PL
Phillip Leff, DO
Creighton University School of Medicine
Scottsdale, AZ
Presenting Author(s)
Phillip Leff, DO1, Elvis J. Arteaga, MD2, Xue Jing Li, MD3, Kenneth S. Zurcher, MD4, Steve Chen, MD5, Moises Nevah Rubin, MD5
1Creighton University School of Medicine, Scottsdale, AZ; 2University of Arizona College of Medicine, Phoenix, AZ; 3University of Arizona College of Medicine, Phoenix VA Medical Center, Phoenix, AZ; 4Vascular & Interventional Partners, Scottsdale, AZ; 5Banner University Medical Center, Phoenix, AZ
Introduction: Portal hypertension can lead to various complications, including ascites, hepatic encephalopathy, and variceal bleeds. The most common variceal bleeds occur in the esophagus. The prevalence of colonic varices is roughly 0.07% and is found in 1% to 8% of patients with cirrhosis.1
Colonic varices, though rare, are another manifestation of portal hypertension, typically found in the rectum and cecum.1, 2 Due to their rarity, there is a general lack of guidelines for treatment.1 This case discusses a patient with descending colonic varix treated with transjugular intrahepatic portosystemic shunt (TIPS) and embolization.
Case Description/Methods: A 45-year-old male with decompensated alcoholic cirrhosis presented to the hospital after an outpatient paracentesis revealed spontaneous bacterial peritonitis. Upon admission, he reported intermittent hematochezia. Initial labs showed a hemoglobin level of 7.1 g/dL. On the fourth day of hospitalization, he developed abdominal pain and bright red blood per rectum, with Hgb dropping from 7.0 g/dL to 5.4 g/dL. He received four units of pRBCs, raising his Hgb to 6.5 g/dL. A flexible sigmoidoscopy revealed a submucosal mass in the descending colon and blood in the descending and sigmoid colon, but no bleeding source was identified.
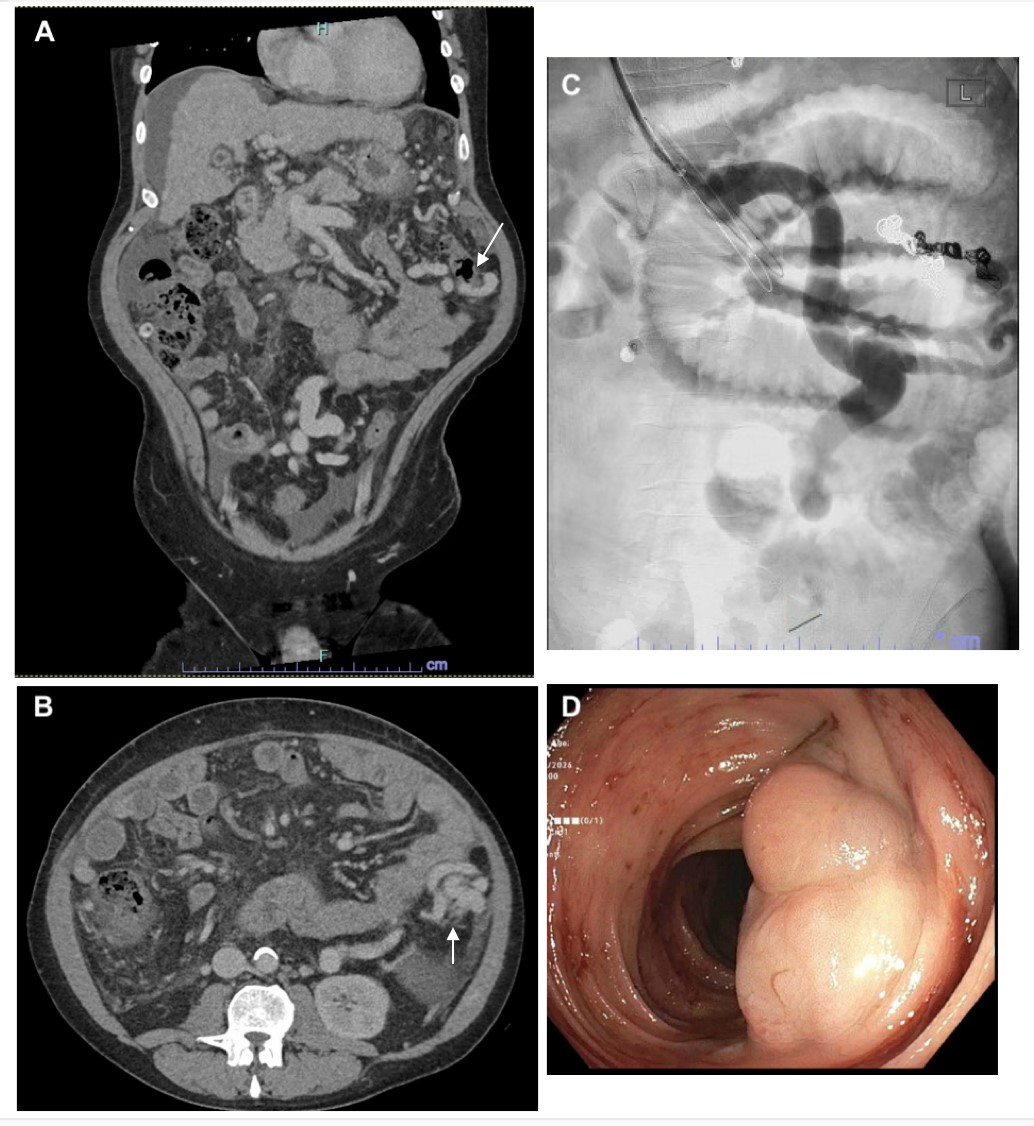
A CT angiogram of the abdomen indicated large varices in the descending colon. The patient underwent a TIPS procedure with a pre-TIPS gradient of 16 mmHg and a post-TIPS gradient of 9 mmHg. During angiography, an inferior mesenteric varix was identified and subsequently treated with coil embolization. Despite this intervention, the patient continued to experience hematochezia. A second coil embolization was performed, which successfully resolved the issue.
Discussion: Treatment options for colonic varices include sclerotherapy, cyanoacrylate injection, TIPS, embolization, and BRTO.3 Our patient developed hematochezia from colonic variceal bleeding while being treated for spontaneous bacterial peritonitis and was treated with TIPS and embolization. The persistence of hematochezia despite initial interventions underscores the complexity of managing colonic varices. Though rare, providers should consider colonic varix in the differential diagnosis for any cirrhotic patient presenting with lower gastrointestinal bleeding.
Disclosures:
Phillip Leff, DO1, Elvis J. Arteaga, MD2, Xue Jing Li, MD3, Kenneth S. Zurcher, MD4, Steve Chen, MD5, Moises Nevah Rubin, MD5. P0783 - An Interesting Case of a Descending Colonic Varix Unresponsive to Transjugular Intrahepatic Portosystemic Shunt Placement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Creighton University School of Medicine, Scottsdale, AZ; 2University of Arizona College of Medicine, Phoenix, AZ; 3University of Arizona College of Medicine, Phoenix VA Medical Center, Phoenix, AZ; 4Vascular & Interventional Partners, Scottsdale, AZ; 5Banner University Medical Center, Phoenix, AZ
Introduction: Portal hypertension can lead to various complications, including ascites, hepatic encephalopathy, and variceal bleeds. The most common variceal bleeds occur in the esophagus. The prevalence of colonic varices is roughly 0.07% and is found in 1% to 8% of patients with cirrhosis.1
Colonic varices, though rare, are another manifestation of portal hypertension, typically found in the rectum and cecum.1, 2 Due to their rarity, there is a general lack of guidelines for treatment.1 This case discusses a patient with descending colonic varix treated with transjugular intrahepatic portosystemic shunt (TIPS) and embolization.
Case Description/Methods: A 45-year-old male with decompensated alcoholic cirrhosis presented to the hospital after an outpatient paracentesis revealed spontaneous bacterial peritonitis. Upon admission, he reported intermittent hematochezia. Initial labs showed a hemoglobin level of 7.1 g/dL. On the fourth day of hospitalization, he developed abdominal pain and bright red blood per rectum, with Hgb dropping from 7.0 g/dL to 5.4 g/dL. He received four units of pRBCs, raising his Hgb to 6.5 g/dL. A flexible sigmoidoscopy revealed a submucosal mass in the descending colon and blood in the descending and sigmoid colon, but no bleeding source was identified.
A CT angiogram of the abdomen indicated large varices in the descending colon. The patient underwent a TIPS procedure with a pre-TIPS gradient of 16 mmHg and a post-TIPS gradient of 9 mmHg. During angiography, an inferior mesenteric varix was identified and subsequently treated with coil embolization. Despite this intervention, the patient continued to experience hematochezia. A second coil embolization was performed, which successfully resolved the issue.
Discussion: Treatment options for colonic varices include sclerotherapy, cyanoacrylate injection, TIPS, embolization, and BRTO.3 Our patient developed hematochezia from colonic variceal bleeding while being treated for spontaneous bacterial peritonitis and was treated with TIPS and embolization. The persistence of hematochezia despite initial interventions underscores the complexity of managing colonic varices. Though rare, providers should consider colonic varix in the differential diagnosis for any cirrhotic patient presenting with lower gastrointestinal bleeding.
Figure: Image A: colonic varix as seen on coronal section of the CTA A/P; Image B: colonix varix as seen on axial section of the CTA A/P; Image C: coil embolization of inferior mesenteric vein; Image D: colonic varix on colonoscopy
Disclosures:
Phillip Leff indicated no relevant financial relationships.
Elvis Arteaga indicated no relevant financial relationships.
Xue Jing Li indicated no relevant financial relationships.
Kenneth Zurcher indicated no relevant financial relationships.
Steve Chen indicated no relevant financial relationships.
Moises Nevah Rubin indicated no relevant financial relationships.
Phillip Leff, DO1, Elvis J. Arteaga, MD2, Xue Jing Li, MD3, Kenneth S. Zurcher, MD4, Steve Chen, MD5, Moises Nevah Rubin, MD5. P0783 - An Interesting Case of a Descending Colonic Varix Unresponsive to Transjugular Intrahepatic Portosystemic Shunt Placement, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
