Sunday Poster Session
Category: GI Bleeding
P0817 - Ectopic Variceal Bleeding and Hemoperitoneum: A Case Report and Management Challenges
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- AB
Ahan Bhatt, MD
Albert Einstein College of Medicine
New York, NY
Presenting Author(s)
Ahan Bhatt, MD1, Fnu Vikash, MD, M.Med1, Donald P. Kotler, MD2, Sunny Patel, MD2
1Albert Einstein College of Medicine, New York, NY; 2Albert Einstein College of Medicine, Bronx, NY
Introduction: Ectopic or extraluminal varices are abnormally dilated veins associated with gastrointestinal mucosa and account for 1 to 5% of variceal bleeds. They are used to describe portosystemic collaterals anywhere else within the abdominal cavity and retroperitoneum beyond the gastroesophageal region.
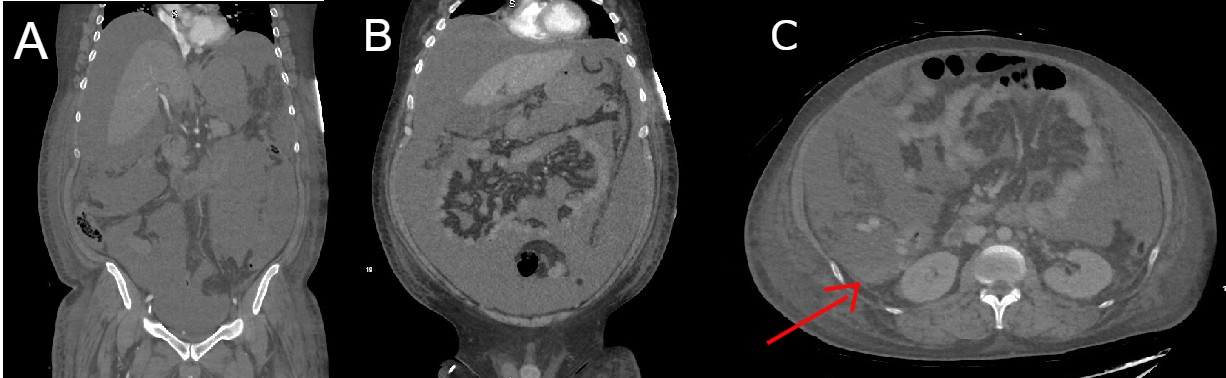
Case Description/Methods: 41-year-old male with past medical history of metabolic syndrome, alcohol use-associated liver cirrhosis complicated by ascites requiring multiple large volume paracentesis in the last 3 months presented to the ED after a witnessed syncope. The most recent LVP was 2 weeks prior to current admission. On admission, the patient's vitals were BP 74/48 mm of Hg, HR 91 bpm, and SpO2 99% on room air. Physical exam showed scleral icterus and protuberant abdomen with a fluid wave. The patient was alert and oriented, without asterixis but with generalized weakness. Hemoglobin was 6.2 g/dL ( >9 g/dL two weeks ago). PT/aPTT was 36.3/49.3 seconds, INR 3.1, and lactate 5.7 mmol/L. Four hours later, the patient's hemoglobin dropped to 5.6 g/dL, and MAP remained below 65 mmHg despite volume resuscitation. DRE negative for GI bleed. Consequently, pressors were started, and the patient was transferred to the medical ICU. The patient underwent a diagnostic tap, revealing grossly bloody fluid concerning for hemoperitoneum. A CT Angio of the abdomen and pelvis with contrast showed large-volume ascites with hemorrhagic fluid adjacent to the right kidney with no active extravasation. The bleeding was likely due to an ectopic varix near the hepatic varices. The patient was deemed not to be a candidate for surgical intervention or IR coil embolization. Massive transfusion protocol, octreotide drip, and three pressors were started. Despite these measures, the patient remained hypotensive and suffered a cardiac arrest within 18 hours of admission.
Discussion: Intra-abdominal variceal bleeds should be suspected in hemodynamically unstable patients who exhibit a rapid increase in ascites, a drop in hematocrit, and a bloody ascitic tap without overt signs of GI bleeding. Management involves maintaining a high index of suspicion, performing an early diagnostic tap and a multidisciplinary case-dependent approach involving GI, IR and Surgery. Treatment options for ectopic bleeds typically include TIPS or surgery. Patients are often unsuitable candidates for life-saving procedures due to multiple comorbidities and are associated with high morbidity and mortality.
Disclosures:
Ahan Bhatt, MD1, Fnu Vikash, MD, M.Med1, Donald P. Kotler, MD2, Sunny Patel, MD2. P0817 - Ectopic Variceal Bleeding and Hemoperitoneum: A Case Report and Management Challenges, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Albert Einstein College of Medicine, New York, NY; 2Albert Einstein College of Medicine, Bronx, NY
Introduction: Ectopic or extraluminal varices are abnormally dilated veins associated with gastrointestinal mucosa and account for 1 to 5% of variceal bleeds. They are used to describe portosystemic collaterals anywhere else within the abdominal cavity and retroperitoneum beyond the gastroesophageal region.
Case Description/Methods: 41-year-old male with past medical history of metabolic syndrome, alcohol use-associated liver cirrhosis complicated by ascites requiring multiple large volume paracentesis in the last 3 months presented to the ED after a witnessed syncope. The most recent LVP was 2 weeks prior to current admission. On admission, the patient's vitals were BP 74/48 mm of Hg, HR 91 bpm, and SpO2 99% on room air. Physical exam showed scleral icterus and protuberant abdomen with a fluid wave. The patient was alert and oriented, without asterixis but with generalized weakness. Hemoglobin was 6.2 g/dL ( >9 g/dL two weeks ago). PT/aPTT was 36.3/49.3 seconds, INR 3.1, and lactate 5.7 mmol/L. Four hours later, the patient's hemoglobin dropped to 5.6 g/dL, and MAP remained below 65 mmHg despite volume resuscitation. DRE negative for GI bleed. Consequently, pressors were started, and the patient was transferred to the medical ICU. The patient underwent a diagnostic tap, revealing grossly bloody fluid concerning for hemoperitoneum. A CT Angio of the abdomen and pelvis with contrast showed large-volume ascites with hemorrhagic fluid adjacent to the right kidney with no active extravasation. The bleeding was likely due to an ectopic varix near the hepatic varices. The patient was deemed not to be a candidate for surgical intervention or IR coil embolization. Massive transfusion protocol, octreotide drip, and three pressors were started. Despite these measures, the patient remained hypotensive and suffered a cardiac arrest within 18 hours of admission.
Discussion: Intra-abdominal variceal bleeds should be suspected in hemodynamically unstable patients who exhibit a rapid increase in ascites, a drop in hematocrit, and a bloody ascitic tap without overt signs of GI bleeding. Management involves maintaining a high index of suspicion, performing an early diagnostic tap and a multidisciplinary case-dependent approach involving GI, IR and Surgery. Treatment options for ectopic bleeds typically include TIPS or surgery. Patients are often unsuitable candidates for life-saving procedures due to multiple comorbidities and are associated with high morbidity and mortality.
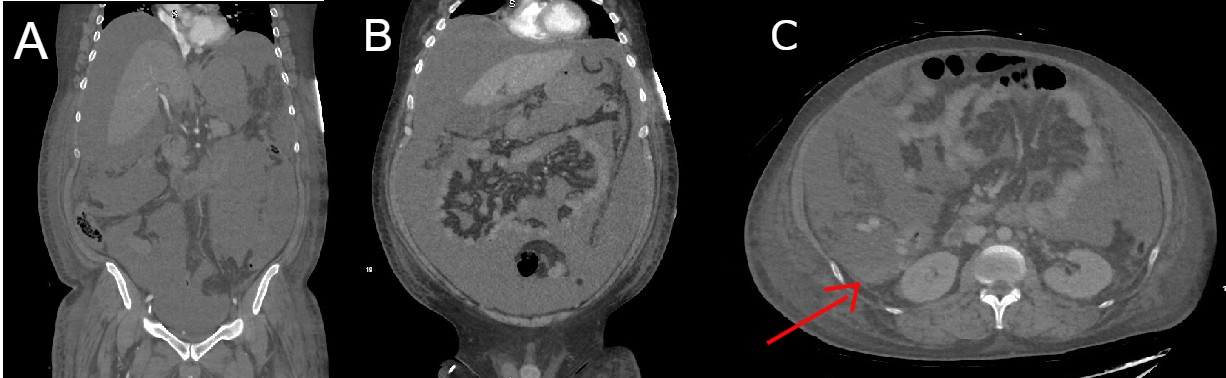
Figure: Images A and B show a coronal section of the abdomen. Image A shows the Ectopic Hepatic Varyx. Images A and B shows Large Volume Ascites. Image C shows a transverse section of the abdomen with hyperintense fluid near the right kidney and hepatic varyx as labeled with red arrow.
Disclosures:
Ahan Bhatt indicated no relevant financial relationships.
Fnu Vikash indicated no relevant financial relationships.
Donald Kotler: EMD Serono – Advisor or Review Panel Member.
Sunny Patel indicated no relevant financial relationships.
Ahan Bhatt, MD1, Fnu Vikash, MD, M.Med1, Donald P. Kotler, MD2, Sunny Patel, MD2. P0817 - Ectopic Variceal Bleeding and Hemoperitoneum: A Case Report and Management Challenges, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

