Sunday Poster Session
Category: GI Bleeding
P0821 - A Case of Splenic Vein Thrombosis, Non-Cirrhotic Portal Hypertension, and Gastric Varices in a Patient With Ovarian Carcinoma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Taylor Bowler, DO
University of Minnesota Medical Center
Minneapolis, MN
Presenting Author(s)
Taylor Bowler, DO1, Lyubov Tiegs, MD2, Bryant Megna, MD1, Nabeel Azeem, MD1
1University of Minnesota Medical Center, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN
Introduction: While ovarian carcinoma has one of the highest rates of venous thromboembolism compared to other solid tumors due to the hypercoagulable nature of the disease, data is limited regarding splenic vein thrombosis in ovarian carcinoma specifically. The development of non-cirrhotic portal hypertension and esophagogastric varices is an uncommon, yet life-threatening complication of splenic vein thrombosis. Recognizing this association between splenic vein thrombosis and non-cirrhotic portal hypertension is critical in reducing morbidity and mortality in patients with hypercoagulable disease secondary to malignancy.
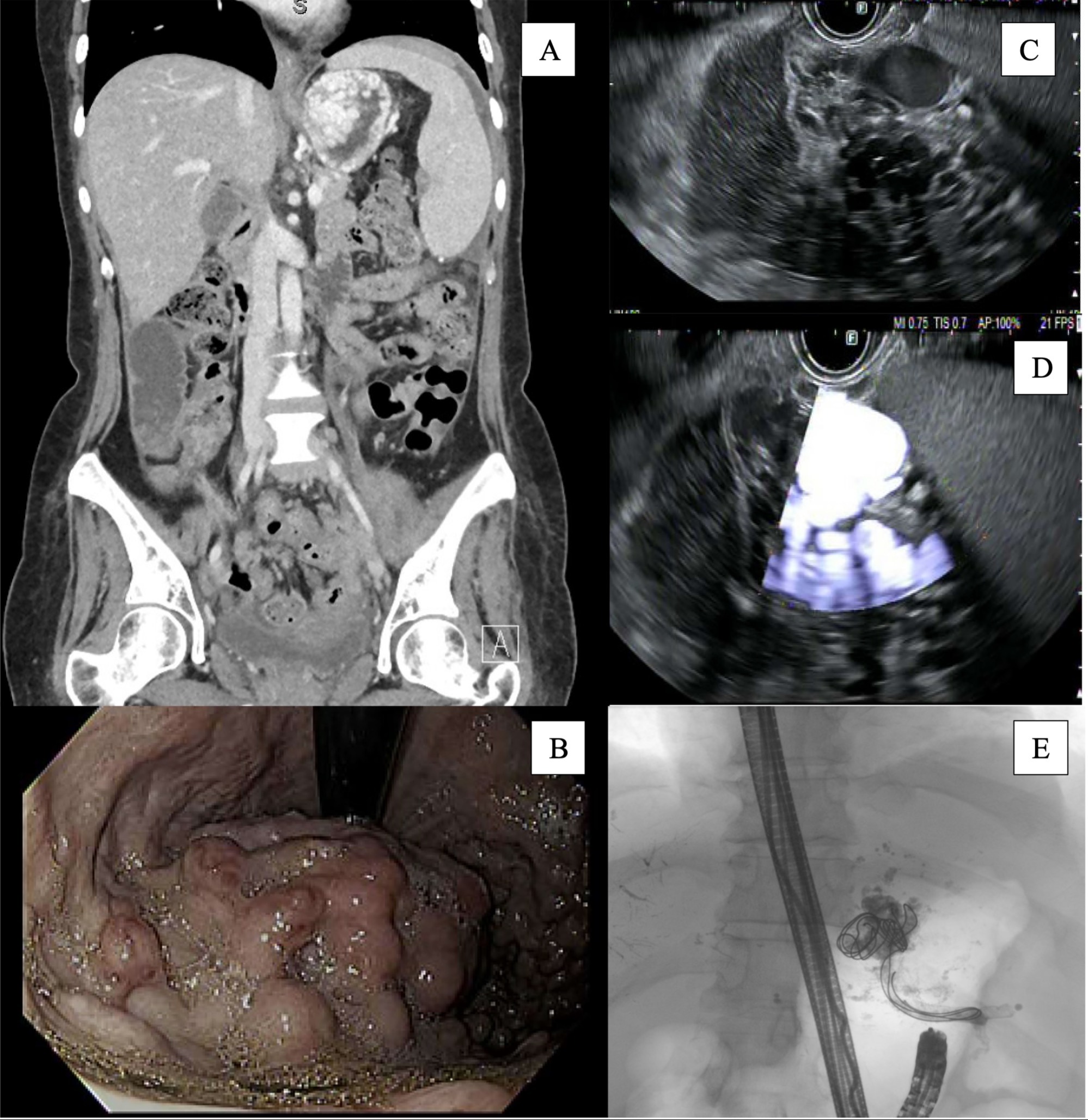
Case Description/Methods: Herein, we present a 45-year-old female with stage IV high grade serous ovarian carcinoma and chronic splenic vein thrombosis on apixaban who presented with abdominal pain and nausea. A CT abdomen/pelvis showed dilated small bowel with stool burden in the colon, mild steatosis without cirrhotic changes in the liver, splenic vein thrombosis and splenomegaly (14.2 cm) (Figure 1A). Treatment was initiated for a presumed small bowel obstruction. 24 hours after hospital admission, the patient developed vomiting with 150 mL of hematemesis. Gastroenterology was then consulted for evaluation. An esophagogastroduodenoscopy showed large > 5 mm esophageal varices and type 2 gastric varices with high-risk stigmata, which were suspected to be the bleeding source (Figure 1B). An endoscopic ultrasound was performed the next day and demonstrated type 2 isolated gastric varices in the fundus, measuring 13.3 mm at the inflow tract as it crossed the gastric wall from the splenic hilum (Figure 1C/D). The largest varix projecting from the splenic hilum was targeted at the stomach wall with successful obliteration using coil-glue (Figure 1E). The apex of the main gastric varix was also targeted with evidence of obliteration. Splenic artery embolization and splenectomy were considered, however a multidisciplinary decision was made to defer interventions due to known splenic metastases with risk of abscess formation. The patient was discharged with plans for repeat EUS to eradicate the remaining variceal bundle.
Discussion: This case highlights that patients with ovarian carcinoma are at risk of splenic vein thrombosis due to the hypercoagulable nature of the disease. Therefore, it is critical to consider the potential sequelae of non-cirrhotic portal hypertension to assure early intervention and mitigate risk of life-threatening gastric variceal hemorrhage as seen in our patient.
Disclosures:
Taylor Bowler, DO1, Lyubov Tiegs, MD2, Bryant Megna, MD1, Nabeel Azeem, MD1. P0821 - A Case of Splenic Vein Thrombosis, Non-Cirrhotic Portal Hypertension, and Gastric Varices in a Patient With Ovarian Carcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota Medical Center, Minneapolis, MN; 2University of Minnesota, Minneapolis, MN
Introduction: While ovarian carcinoma has one of the highest rates of venous thromboembolism compared to other solid tumors due to the hypercoagulable nature of the disease, data is limited regarding splenic vein thrombosis in ovarian carcinoma specifically. The development of non-cirrhotic portal hypertension and esophagogastric varices is an uncommon, yet life-threatening complication of splenic vein thrombosis. Recognizing this association between splenic vein thrombosis and non-cirrhotic portal hypertension is critical in reducing morbidity and mortality in patients with hypercoagulable disease secondary to malignancy.
Case Description/Methods: Herein, we present a 45-year-old female with stage IV high grade serous ovarian carcinoma and chronic splenic vein thrombosis on apixaban who presented with abdominal pain and nausea. A CT abdomen/pelvis showed dilated small bowel with stool burden in the colon, mild steatosis without cirrhotic changes in the liver, splenic vein thrombosis and splenomegaly (14.2 cm) (Figure 1A). Treatment was initiated for a presumed small bowel obstruction. 24 hours after hospital admission, the patient developed vomiting with 150 mL of hematemesis. Gastroenterology was then consulted for evaluation. An esophagogastroduodenoscopy showed large > 5 mm esophageal varices and type 2 gastric varices with high-risk stigmata, which were suspected to be the bleeding source (Figure 1B). An endoscopic ultrasound was performed the next day and demonstrated type 2 isolated gastric varices in the fundus, measuring 13.3 mm at the inflow tract as it crossed the gastric wall from the splenic hilum (Figure 1C/D). The largest varix projecting from the splenic hilum was targeted at the stomach wall with successful obliteration using coil-glue (Figure 1E). The apex of the main gastric varix was also targeted with evidence of obliteration. Splenic artery embolization and splenectomy were considered, however a multidisciplinary decision was made to defer interventions due to known splenic metastases with risk of abscess formation. The patient was discharged with plans for repeat EUS to eradicate the remaining variceal bundle.
Discussion: This case highlights that patients with ovarian carcinoma are at risk of splenic vein thrombosis due to the hypercoagulable nature of the disease. Therefore, it is critical to consider the potential sequelae of non-cirrhotic portal hypertension to assure early intervention and mitigate risk of life-threatening gastric variceal hemorrhage as seen in our patient.
Figure: Figure 1. A. Computed tomography of the abdomen/pelvis demonstrating splenomegaly and dilated collaterals in the proximal stomach. B. Upper endoscopy with high-risk variceal stigmata (red wale signs). C. Endoscopic ultrasound sonographic image of the variceal bundle in gastric wall. D. Doppler image of the variceal bundle demonstrating significant inflow. E. Fluoroscopic image post-embolization with visible vascular coils and lipiodol mixture within the body of the largest variceal bundle as well as the inflow tract from the splenic hilum.
Disclosures:
Taylor Bowler indicated no relevant financial relationships.
Lyubov Tiegs indicated no relevant financial relationships.
Bryant Megna indicated no relevant financial relationships.
Nabeel Azeem: Boston Scientific – Consultant.
Taylor Bowler, DO1, Lyubov Tiegs, MD2, Bryant Megna, MD1, Nabeel Azeem, MD1. P0821 - A Case of Splenic Vein Thrombosis, Non-Cirrhotic Portal Hypertension, and Gastric Varices in a Patient With Ovarian Carcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
