Sunday Poster Session
Category: GI Bleeding
P0823 - Rare Left-sided Portal Hypertension: Recurrent Gastric Variceal Bleeding Due to Extrinsic Splenic Vein Compression from Pancreatic Tail Adenocarcinoma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E

Sami Mesgun, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University, OH
Presenting Author(s)
Sami Mesgun, MD1, Adily Elmi, MD, MPH2, Jenny Jan, MD3, Vibhu Chittajallu, MD4, Emad Mansoor, MD5
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2University Hospitals, Cleveland Medical Center, Cleveland Heights, OH; 3University Hospitals Cleveland Medical Center, Cleveland, OH; 4West Virginia University, Cleveland, OH; 5Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Gastric varices (GV) are less common than esophageal varices, exhibit higher rates of rebleeding, and carry an increased risk of mortality. Isolated GVs are typically found in the fundus and observed in only 1.6% of patients with GV. Herein, we describe a rare case of recurrent gastric variceal bleeding due to splenic vein compression by a pancreatic tail adenocarcinoma.
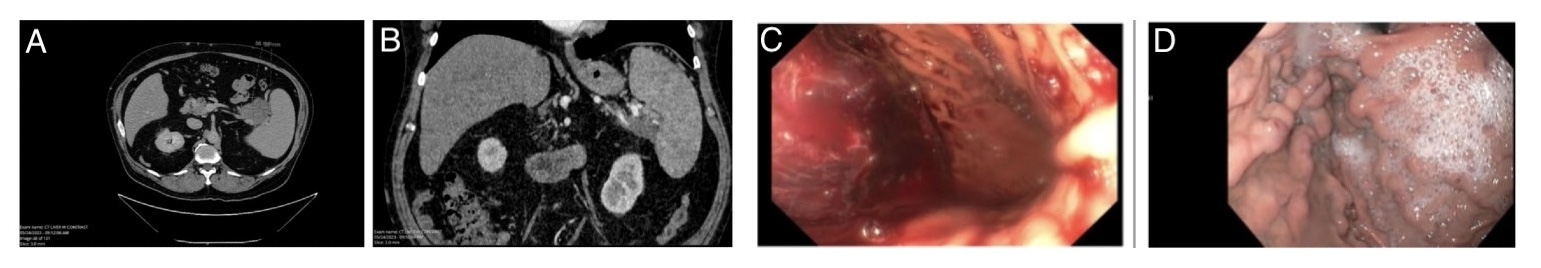
Case Description/Methods: A 64-year-old male was initially referred to outpatient gastroenterology for melena and acute anemia. He was evaluated with esophagogastroduodenoscopy (EGD) which showed non-bleeding type 1 gastroesophageal varices (GOV1) and type 1 isolated gastric varices (IGV1) without high-risk stigmata. Given these findings, computed tomography (CT) scan of the abdomen was obtained and showed a 5.9 cm mass in the pancreatic tail that was obstructing the splenic vein, leading to GVs (Figure 1A and 1B). He was diagnosed with pancreatic adenocarcinoma by endoscopic-ultrasound guided biopsy. Three months later, while still undergoing neoadjuvant chemotherapy prior to surgical resection, he presented with recurrent melena and blood loss anemia. Labs showed a hemoglobin of 5.3 and a BUN to creatinine ratio of 48. He was admitted to the intensive care unit for hemorrhagic shock. EGD showed fresh and clotted blood in the gastric fundus and cardia which obscured visualization and was unable to be cleared. (Figure 1C and 1D). He was transferred to a tertiary care center for further care where repeat EGD re-demonstrated large GOV1 and IGV1. As bleeding had stopped, lack of high risk-stigmata, and extent of gastric varices, no endoscopic intervention was performed. Instead, he underwent urgent distal pancreatectomy and splenectomy with Surgical Oncology with no further bleeding.
Discussion: This is a case of left-sided portal hypertension caused by splenic vein occlusion due to extrinsic compression by an adenocarcinoma of the pancreatic tail. Obstructed blood flow in the proximal splenic vein leads to increased pressure in collateral vessels in the stomach and isolated GVs form. Life-threatening GV bleeding can occur, and endoscopic management can be challenging based on location and extent of GVs. Additionally, many patients with pancreatic adenocarcinoma will undergo neo-adjuvant chemotherapy prior to surgical resection. Our patient’s chemotherapy course was unfortunately interrupted by recurrent life-threatening GV bleeding and urgent surgical resection was performed.
Disclosures:
Sami Mesgun, MD1, Adily Elmi, MD, MPH2, Jenny Jan, MD3, Vibhu Chittajallu, MD4, Emad Mansoor, MD5. P0823 - Rare Left-sided Portal Hypertension: Recurrent Gastric Variceal Bleeding Due to Extrinsic Splenic Vein Compression from Pancreatic Tail Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2University Hospitals, Cleveland Medical Center, Cleveland Heights, OH; 3University Hospitals Cleveland Medical Center, Cleveland, OH; 4West Virginia University, Cleveland, OH; 5Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Gastric varices (GV) are less common than esophageal varices, exhibit higher rates of rebleeding, and carry an increased risk of mortality. Isolated GVs are typically found in the fundus and observed in only 1.6% of patients with GV. Herein, we describe a rare case of recurrent gastric variceal bleeding due to splenic vein compression by a pancreatic tail adenocarcinoma.
Case Description/Methods: A 64-year-old male was initially referred to outpatient gastroenterology for melena and acute anemia. He was evaluated with esophagogastroduodenoscopy (EGD) which showed non-bleeding type 1 gastroesophageal varices (GOV1) and type 1 isolated gastric varices (IGV1) without high-risk stigmata. Given these findings, computed tomography (CT) scan of the abdomen was obtained and showed a 5.9 cm mass in the pancreatic tail that was obstructing the splenic vein, leading to GVs (Figure 1A and 1B). He was diagnosed with pancreatic adenocarcinoma by endoscopic-ultrasound guided biopsy. Three months later, while still undergoing neoadjuvant chemotherapy prior to surgical resection, he presented with recurrent melena and blood loss anemia. Labs showed a hemoglobin of 5.3 and a BUN to creatinine ratio of 48. He was admitted to the intensive care unit for hemorrhagic shock. EGD showed fresh and clotted blood in the gastric fundus and cardia which obscured visualization and was unable to be cleared. (Figure 1C and 1D). He was transferred to a tertiary care center for further care where repeat EGD re-demonstrated large GOV1 and IGV1. As bleeding had stopped, lack of high risk-stigmata, and extent of gastric varices, no endoscopic intervention was performed. Instead, he underwent urgent distal pancreatectomy and splenectomy with Surgical Oncology with no further bleeding.
Discussion: This is a case of left-sided portal hypertension caused by splenic vein occlusion due to extrinsic compression by an adenocarcinoma of the pancreatic tail. Obstructed blood flow in the proximal splenic vein leads to increased pressure in collateral vessels in the stomach and isolated GVs form. Life-threatening GV bleeding can occur, and endoscopic management can be challenging based on location and extent of GVs. Additionally, many patients with pancreatic adenocarcinoma will undergo neo-adjuvant chemotherapy prior to surgical resection. Our patient’s chemotherapy course was unfortunately interrupted by recurrent life-threatening GV bleeding and urgent surgical resection was performed.
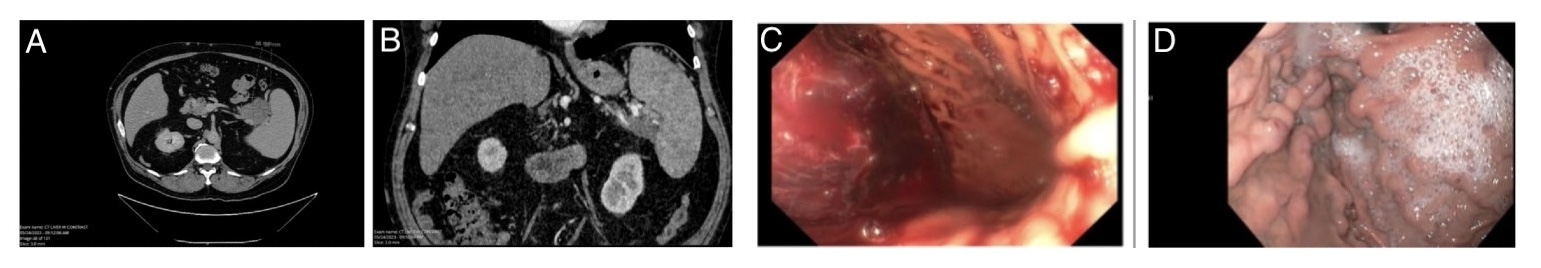
Figure: Figure 1: A and B) CT Abdomen with incidental finding of a pancreatic tail mass extrinsically compressing splenic vein and splenomegaly. C) Initial EGD with evidence of active bleeding. D) Isolated gastric varices located in the fundus.
Disclosures:
Sami Mesgun indicated no relevant financial relationships.
Adily Elmi indicated no relevant financial relationships.
Jenny Jan indicated no relevant financial relationships.
Vibhu Chittajallu indicated no relevant financial relationships.
Emad Mansoor: Lilly – Speakers Bureau. Takeda – Speakers Bureau.
Sami Mesgun, MD1, Adily Elmi, MD, MPH2, Jenny Jan, MD3, Vibhu Chittajallu, MD4, Emad Mansoor, MD5. P0823 - Rare Left-sided Portal Hypertension: Recurrent Gastric Variceal Bleeding Due to Extrinsic Splenic Vein Compression from Pancreatic Tail Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
