Sunday Poster Session
Category: IBD
P0853 - Low Incidence of Macular Edema in Patients in the Etrasimod Clinical Program
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Marla Dubinsky, MD
Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Marla C. Dubinsky, MD1, Joseph Wu, PhD2, Aoibhinn McDonnell, PhD3, Krisztina Lazin, MD4, Martina Goetsch, MD4, Diogo Branquinho, MD, MSc5, Irene Modesto, MD5, Alessandro Armuzzi, MD, PhD6
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Pfizer Inc., Cambridge, MA; 3Pfizer Ltd., Sandwich, England, United Kingdom; 4Pfizer AG, Zürich, Zurich, Switzerland; 5Pfizer Inc., New York, NY; 6IBD Unit, IRCCS Humanitas Research Hospital, Rozzano, Humanitas University, Pieve Emanuele, Milan, Lombardia, Italy
Introduction: Sphingosine 1-phosphate (S1P) receptor modulators have been associated with an increased risk of macular edema.1 Etrasimod is an oral, once-daily (QD), selective S1P1,4,5 receptor modulator for the treatment of moderately to severely active ulcerative colitis (UC) and is in development for the treatment of other immune-mediated inflammatory diseases.
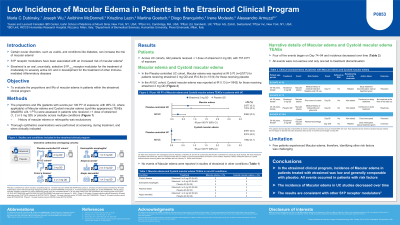
Methods: We assessed the proportions and incidence rates (IRs; patients with events per 100 patient-years [PY] of exposure) of Macular edema and Cystoid macular edema in a comprehensive analysis of safety data from the etrasimod clinical program. UC data were analyzed in two cohorts: Placebo-controlled UC (completed phase [ph] 2 OASIS, ph 3 ELEVATE UC 52 and ELEVATE UC 12) and All UC (patients treated with etrasimod in the Placebo-controlled UC plus open-label extension [OLE] studies; completed ph 2 OASIS OLE and ongoing ph 3 ELEVATE UC and ES101002 OLE studies, both datacut at January 31, 2022). Data from completed ph 2 studies in Crohn’s disease (CULTIVATE substudy A) and placebo-controlled studies in eosinophilic esophagitis (VOYAGE), alopecia areata, and atopic dermatitis (ADVISE) were also analyzed.
Results: Across the etrasimod UC clinical program, 942 patients received ≥ 1 dose of etrasimod 2 mg QD, with 757.9 PY of exposure. In the Placebo-controlled UC cohort, Macular edema was reported in two patients (0.3%; IR 0.70) receiving etrasimod 2 mg QD (one patient with long-term corticosteroid use in ELEVATE UC 52 and one patient with prior uveitis in ELEVATE UC 12, which was not considered clinically significant by the investigator) and one patient (0.3%; IR 0.84) receiving placebo (ELEVATE UC 12). In the All UC cohort, one patient (0.1%; IR 0.13) receiving etrasimod 2 mg QD during the ELEVATE UC OLE reported two events of Cystoid macular edema (Table). Four of five Macular edema events began at Days 74–94, all were non-serious and only one event led to treatment discontinuation. No events of Macular edema were reported in studies of etrasimod in other indications (Table).
Discussion: The incidence of Macular edema in patients treated with etrasimod in the clinical program was low and generally comparable with placebo. These results are consistent with other S1P receptor modulators1 and provide clinically relevant information on events of Macular edema.
Reference:
Bencardino S et al. J Clin Med 2023; 12: 5014.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Marla C. Dubinsky, MD1, Joseph Wu, PhD2, Aoibhinn McDonnell, PhD3, Krisztina Lazin, MD4, Martina Goetsch, MD4, Diogo Branquinho, MD, MSc5, Irene Modesto, MD5, Alessandro Armuzzi, MD, PhD6. P0853 - Low Incidence of Macular Edema in Patients in the Etrasimod Clinical Program, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai, New York, NY; 2Pfizer Inc., Cambridge, MA; 3Pfizer Ltd., Sandwich, England, United Kingdom; 4Pfizer AG, Zürich, Zurich, Switzerland; 5Pfizer Inc., New York, NY; 6IBD Unit, IRCCS Humanitas Research Hospital, Rozzano, Humanitas University, Pieve Emanuele, Milan, Lombardia, Italy
Introduction: Sphingosine 1-phosphate (S1P) receptor modulators have been associated with an increased risk of macular edema.1 Etrasimod is an oral, once-daily (QD), selective S1P1,4,5 receptor modulator for the treatment of moderately to severely active ulcerative colitis (UC) and is in development for the treatment of other immune-mediated inflammatory diseases.
Methods: We assessed the proportions and incidence rates (IRs; patients with events per 100 patient-years [PY] of exposure) of Macular edema and Cystoid macular edema in a comprehensive analysis of safety data from the etrasimod clinical program. UC data were analyzed in two cohorts: Placebo-controlled UC (completed phase [ph] 2 OASIS, ph 3 ELEVATE UC 52 and ELEVATE UC 12) and All UC (patients treated with etrasimod in the Placebo-controlled UC plus open-label extension [OLE] studies; completed ph 2 OASIS OLE and ongoing ph 3 ELEVATE UC and ES101002 OLE studies, both datacut at January 31, 2022). Data from completed ph 2 studies in Crohn’s disease (CULTIVATE substudy A) and placebo-controlled studies in eosinophilic esophagitis (VOYAGE), alopecia areata, and atopic dermatitis (ADVISE) were also analyzed.
Results: Across the etrasimod UC clinical program, 942 patients received ≥ 1 dose of etrasimod 2 mg QD, with 757.9 PY of exposure. In the Placebo-controlled UC cohort, Macular edema was reported in two patients (0.3%; IR 0.70) receiving etrasimod 2 mg QD (one patient with long-term corticosteroid use in ELEVATE UC 52 and one patient with prior uveitis in ELEVATE UC 12, which was not considered clinically significant by the investigator) and one patient (0.3%; IR 0.84) receiving placebo (ELEVATE UC 12). In the All UC cohort, one patient (0.1%; IR 0.13) receiving etrasimod 2 mg QD during the ELEVATE UC OLE reported two events of Cystoid macular edema (Table). Four of five Macular edema events began at Days 74–94, all were non-serious and only one event led to treatment discontinuation. No events of Macular edema were reported in studies of etrasimod in other indications (Table).
Discussion: The incidence of Macular edema in patients treated with etrasimod in the clinical program was low and generally comparable with placebo. These results are consistent with other S1P receptor modulators1 and provide clinically relevant information on events of Macular edema.
Reference:
Bencardino S et al. J Clin Med 2023; 12: 5014.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Marla Dubinsky: AbbVie – Consultant. Abivax – Consultant. Arena – Consultant. AstraZeneca – Consultant. Bristol Myers Squibb – Consultant. Celgene – Consultant. Eli Lilly – Consultant. Genentech – Consultant. Gilead – Consultant. Janssen – Consultant. Pfizer Inc – Consultant. Prometheus Labs – Consultant. Takeda – Consultant.
Joseph Wu: Pfizer Inc – Employee, Stock Options.
Aoibhinn McDonnell: Pfizer Inc – Stock Options. Pfizer Ltd – Employee.
Krisztina Lazin: Pfizer AG – Employee. Pfizer Inc – Stock Options.
Martina Goetsch: Pfizer AG – Employee, Stock Options.
Diogo Branquinho: Pfizer Inc – Employee, Stock Options.
Irene Modesto: Pfizer Inc – Employee, Stock Options.
Alessandro Armuzzi: AbbVie – Consultant, Speakers Bureau. Allergan – Advisory Committee/Board Member, Consultant. Amgen – Consultant, Speakers Bureau. Arena – Advisory Committee/Board Member, Consultant. Biogen – Consultant, Grant/Research Support, Speakers Bureau. Boehringer Ingleheim – Consultant. Bristol-Myers Squibb – Consultant, Grant/Research Support. Celltrion – Consultant. Eli Lilly – Consultant, Speakers Bureau. Ferring Pharmaceuticals – Consultant, Speakers Bureau. Galapagos – Consultant, Speakers Bureau. Gilead Sciences – Consultant, Speakers Bureau. Janssen – Consultant, Speakers Bureau. Lionhealth – Consultant, Speakers Bureau. Mitsubishi Tanabe – Speakers Bureau. MSD – Consultant, Grant/Research Support, Speakers Bureau. Mylan – Consultant. Nestle – Consultant. Novartis – Speakers Bureau. Pfizer Inc – Consultant, Grant/Research Support, Speakers Bureau. Roche – Consultant, Speakers Bureau. Samsung Bioepis – Consultant, Speakers Bureau. Sandoz – Consultant, Speakers Bureau. Takeda – Consultant, Grant/Research Support, Speakers Bureau. TiGenix – Speakers Bureau. Tillots – Consultant.
Marla C. Dubinsky, MD1, Joseph Wu, PhD2, Aoibhinn McDonnell, PhD3, Krisztina Lazin, MD4, Martina Goetsch, MD4, Diogo Branquinho, MD, MSc5, Irene Modesto, MD5, Alessandro Armuzzi, MD, PhD6. P0853 - Low Incidence of Macular Edema in Patients in the Etrasimod Clinical Program, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
