Sunday Poster Session
Category: IBD
P0861 - Continuing or Discontinuing Mesalamine in Crohn’s Disease? A Multinational, Propensity-Matched, Retrospective Cohort Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- FA
Feyzullah Aksan, MD
Renaissance School of Medicine, Stony Brook University
Port Jefferson Station, NY
Presenting Author(s)
Feyzullah Aksan, MD1, Lokman Hekim Tanriverdi, PhD2, Layla Barrera, DO3, Thomas Ullman, MD4
1Renaissance School of Medicine, Stony Brook University, Port Jefferson Station, NY; 2Inonu University School of Medicine, Malatya, Malatya, Turkey; 3Stony Brook University Hospital, Port Jefferson Station, NY; 4Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY
Introduction: Recent guidelines do not recommend mesalamine (5ASA) for Crohn’s disease (CD), but it is still widely prescribed. Some experts suggest 5ASA might be effective in mild to moderate colonic CD. Our retrospective study explores 5ASA's role in CD and colonic subtypes.
Methods: We used TriNetX, a multi-institutional database, for our retrospective cohort study on 5ASA effectiveness in CD. CD patients before January 1, 2023, were split into two groups: all CD patients (allCD) and colonic CD patients (colonic). Using ICD-10 codes, we created cohorts for each group: 5ASA users and non-users post-index event (allCD or colonic CD diagnosis). Exclusions included prior CD-related surgeries, abscesses or fistulas within the last 3 months, and use of advanced treatments or steroids within the last 3 months. 1:1 propensity score matching (PSM) was done based on age, gender, race, comorbid conditions, and other CD medications. We compared 5-year mortality, IBD-related surgeries, CD complications, steroid use, and healthcare resource utilization (HRU, inpatient/outpatient visits) using Hazard Ratios (HR) and 95% Confidence Intervals (CI), with significance α < 0.05
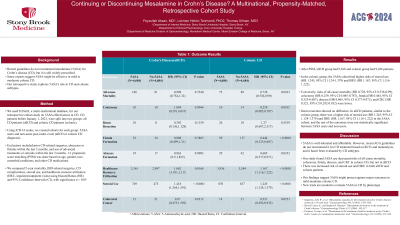
Results: After PSM, allCD group had 9,368 and colonic group had 9,286 patients. In the colonic group, the 5ASA cohort had higher risks of steroid use (HR 1.245, 95% CI 1.124-1.379) and HRU (HR 1.167, 95% CI 1.116-1.222). Conversely, risks of all-cause mortality (HR 0.728, 95% CI 0.536-0.99), colectomy (HR 0.259, 95% CI 0.085-0.787), fistula (HR 0.444, 95% CI 0.325-0.607), abscess (HR 0.605, 95% CI 0.377-0.971), and CRC (HR 0.521, 95% CI 0.292-0.932) were lower. Ileum resection showed no difference. In allCD patients, similar to the colonic group, there was a higher risk of steroid use (HR 1.245, 95% CI 1.124-1.379) and HRU (HR 1.167, 95% CI 1.116-1.222) in the 5ASA cohort, and the rest of the outcomes were not statistically significant between 5ASA users and non-users.
Discussion: 5ASA is well-tolerated and affordable. However, recent ACG guidelines do not recommend it for CD treatment based on RCTs and metanalysis, and it hasn't been evaluated by CD subtypes. Our study found 5ASA use decreased risks of all-cause mortality, colectomy, fistula, abscess, and CRC in colonic CD, but not in allCD. There was increased risk of steroid use and HRU in both allCD and colonic patients. Our findings suggest 5ASA might protect against major outcomes in mild-moderate colonic CD. New trials are needed to evaluate 5ASA in CD by phenotype
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Feyzullah Aksan, MD1, Lokman Hekim Tanriverdi, PhD2, Layla Barrera, DO3, Thomas Ullman, MD4. P0861 - Continuing or Discontinuing Mesalamine in Crohn’s Disease? A Multinational, Propensity-Matched, Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Renaissance School of Medicine, Stony Brook University, Port Jefferson Station, NY; 2Inonu University School of Medicine, Malatya, Malatya, Turkey; 3Stony Brook University Hospital, Port Jefferson Station, NY; 4Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY
Introduction: Recent guidelines do not recommend mesalamine (5ASA) for Crohn’s disease (CD), but it is still widely prescribed. Some experts suggest 5ASA might be effective in mild to moderate colonic CD. Our retrospective study explores 5ASA's role in CD and colonic subtypes.
Methods: We used TriNetX, a multi-institutional database, for our retrospective cohort study on 5ASA effectiveness in CD. CD patients before January 1, 2023, were split into two groups: all CD patients (allCD) and colonic CD patients (colonic). Using ICD-10 codes, we created cohorts for each group: 5ASA users and non-users post-index event (allCD or colonic CD diagnosis). Exclusions included prior CD-related surgeries, abscesses or fistulas within the last 3 months, and use of advanced treatments or steroids within the last 3 months. 1:1 propensity score matching (PSM) was done based on age, gender, race, comorbid conditions, and other CD medications. We compared 5-year mortality, IBD-related surgeries, CD complications, steroid use, and healthcare resource utilization (HRU, inpatient/outpatient visits) using Hazard Ratios (HR) and 95% Confidence Intervals (CI), with significance α < 0.05
Results: After PSM, allCD group had 9,368 and colonic group had 9,286 patients. In the colonic group, the 5ASA cohort had higher risks of steroid use (HR 1.245, 95% CI 1.124-1.379) and HRU (HR 1.167, 95% CI 1.116-1.222). Conversely, risks of all-cause mortality (HR 0.728, 95% CI 0.536-0.99), colectomy (HR 0.259, 95% CI 0.085-0.787), fistula (HR 0.444, 95% CI 0.325-0.607), abscess (HR 0.605, 95% CI 0.377-0.971), and CRC (HR 0.521, 95% CI 0.292-0.932) were lower. Ileum resection showed no difference. In allCD patients, similar to the colonic group, there was a higher risk of steroid use (HR 1.245, 95% CI 1.124-1.379) and HRU (HR 1.167, 95% CI 1.116-1.222) in the 5ASA cohort, and the rest of the outcomes were not statistically significant between 5ASA users and non-users.
Discussion: 5ASA is well-tolerated and affordable. However, recent ACG guidelines do not recommend it for CD treatment based on RCTs and metanalysis, and it hasn't been evaluated by CD subtypes. Our study found 5ASA use decreased risks of all-cause mortality, colectomy, fistula, abscess, and CRC in colonic CD, but not in allCD. There was increased risk of steroid use and HRU in both allCD and colonic patients. Our findings suggest 5ASA might protect against major outcomes in mild-moderate colonic CD. New trials are needed to evaluate 5ASA in CD by phenotype
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Feyzullah Aksan indicated no relevant financial relationships.
Lokman Hekim Tanriverdi indicated no relevant financial relationships.
Layla Barrera indicated no relevant financial relationships.
Thomas Ullman: BMS – Consultant. Pfizer – Advisor or Review Panel Member, Grant/Research Support.
Feyzullah Aksan, MD1, Lokman Hekim Tanriverdi, PhD2, Layla Barrera, DO3, Thomas Ullman, MD4. P0861 - Continuing or Discontinuing Mesalamine in Crohn’s Disease? A Multinational, Propensity-Matched, Retrospective Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

