Sunday Poster Session
Category: IBD
P0894 - Bidirectional Causal Link Between Type 2 Diabetes Mellitus and Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis of Mendelian Randomization Studies
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- PG
Priyatham Gurram, MD
Central Michigan University College of Medicine
Saginaw, MI
Presenting Author(s)
Priyatham Gurram, MD1, Shravya K. Kokkula, MBBS2, Sricharan Chiluveru, MBBS3, Moulika kari, MBBS4, Dayana shre Narayana Swamy, MBBS5, Akhila Reddy Radhareddy, MBBS6, Yamini Katamreddy, MD7, George Mathew Mukalil, MD8, Rupak Desai, MBBS9
1Central Michigan University College of Medicine, Saginaw, MI; 2Dr. Vasantrao Pawar Medical College, Hospital and Research Centre, Nashik, Maharashtra, India; 3Alluri Sitarama Raju Academy of Medical Sciences, Malkapuram, Andhra Pradesh, India; 4Kamineni Institute of Medical Sciences, Narketpalle, Telangana, India; 5Mysore Medical College and Research Institute, Mysore, Karnataka, India; 6MediCiti Institute of Medical Sciences, Medchal, Telangana, India; 7West Anaheim Medical Center, Anaheim, CA; 8Central Michigan University, Saginaw, MI; 9Outcomes Research, Atlanta, GA
Introduction: Inflammatory Bowel Disease (IBD) and Type 2 Diabetes Mellitus (T2DM) are chronic conditions that significantly impact public health. Emerging evidence suggests a relationship between IBD and T2DM, with each potentially influencing the risk of the other. Mendelian Randomization (MR) uses genetic variants to infer causal relationships, minimizing confounding and reverse causation biases. This meta-analysis evaluates the bidirectional causal association between IBD and T2DM through MR studies.
Methods: We systematically searched PubMed, Scholar and Scopus for studies evaluating the association between T2DM and IBD [Ulcerative colitis (UC) and Crohn’s disease (CD)] using MR analysis until June 2024. We included studies which used SNP sources T2DKP, GWAS mahajan et al 2018, GERA, UKB, DIAGRAM, and MRICU for T2DM and FinnGen, GWAS liu et al 2015, and IIBDGC for IBD, UC and CD. Random effects models were used for pooled odds ratios (OR). Heterogeneity was assessed using I2 statistics and a leave one-out sensitivity analysis was performed.
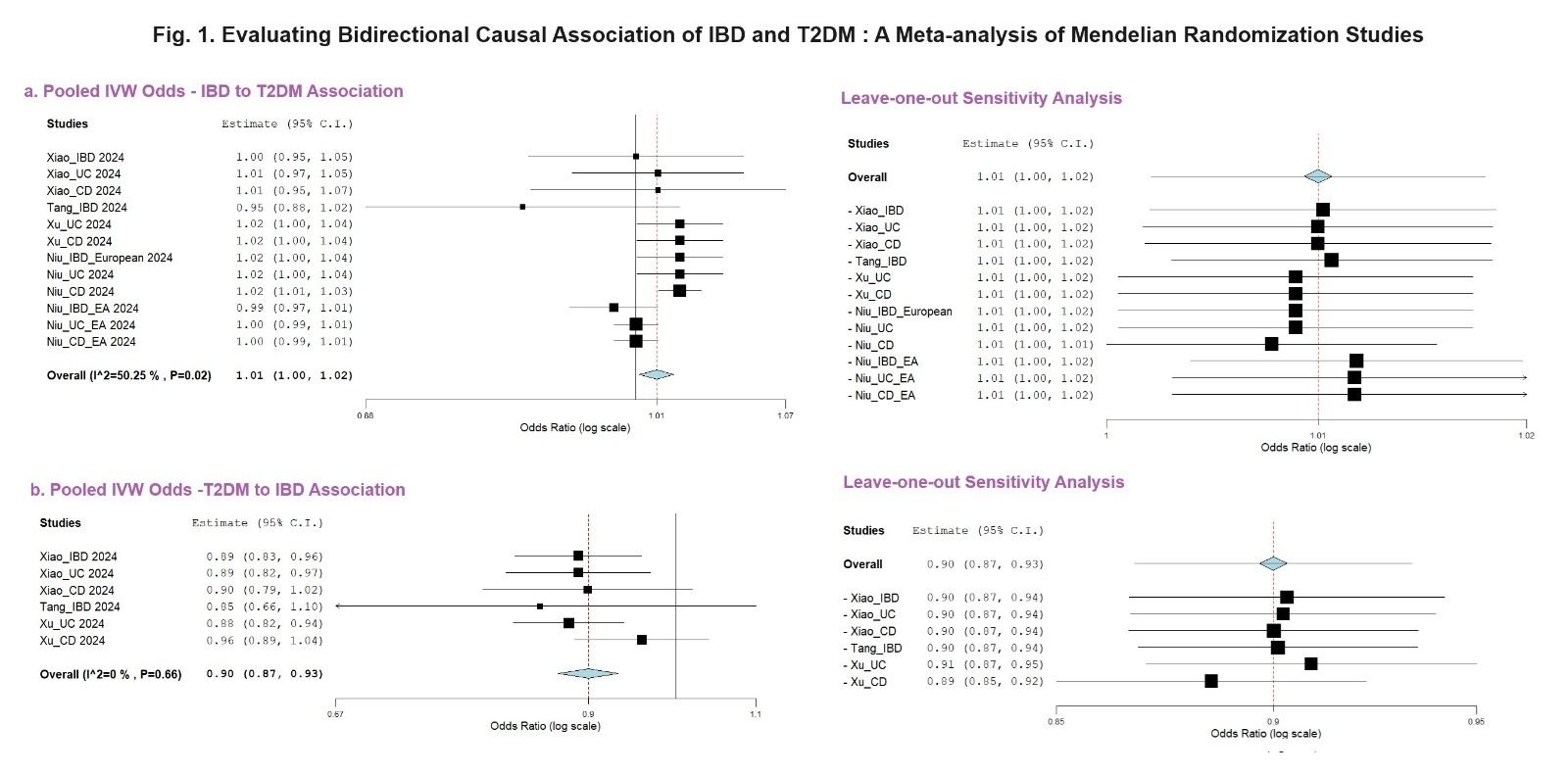
Results: In the 4 studies included, 271657 SNPs were studied mostly using european and east Asian ancestries. In Our analysis the pooled odds of inverse variance weighted method showed that T2DM decreases the risk of overall IBD (OR: 0.90, 95%CI - 0.87 0.93, P < 0.01;I2 =0%), while the overall IBD increases the risk of T2DM (OR: 1.01, 95%CI - 1.00 1.02, P= 0.02; I2=50.25%). A leave-one-out sensitivity analysis demonstrated that no single study significantly influenced the overall results. In a subgroup analysis either IBD or UC or CD do not increase the risk of T2DM (p=0.94, p=0.1 and p=0.07 respectively).
Discussion: The results of the bidirectional MR meta-analysis suggest that presence of T2DM decreases the risk of IBD which may be related to the use of anti-diabetic medications. Conversely, the occurrence of IBD increases the risk of T2DM. This association between T2DM and IBD/UC/CD may be related to multiple immune responses and changes in metabolic pathways.
Disclosures:
Priyatham Gurram, MD1, Shravya K. Kokkula, MBBS2, Sricharan Chiluveru, MBBS3, Moulika kari, MBBS4, Dayana shre Narayana Swamy, MBBS5, Akhila Reddy Radhareddy, MBBS6, Yamini Katamreddy, MD7, George Mathew Mukalil, MD8, Rupak Desai, MBBS9. P0894 - Bidirectional Causal Link Between Type 2 Diabetes Mellitus and Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis of Mendelian Randomization Studies, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Central Michigan University College of Medicine, Saginaw, MI; 2Dr. Vasantrao Pawar Medical College, Hospital and Research Centre, Nashik, Maharashtra, India; 3Alluri Sitarama Raju Academy of Medical Sciences, Malkapuram, Andhra Pradesh, India; 4Kamineni Institute of Medical Sciences, Narketpalle, Telangana, India; 5Mysore Medical College and Research Institute, Mysore, Karnataka, India; 6MediCiti Institute of Medical Sciences, Medchal, Telangana, India; 7West Anaheim Medical Center, Anaheim, CA; 8Central Michigan University, Saginaw, MI; 9Outcomes Research, Atlanta, GA
Introduction: Inflammatory Bowel Disease (IBD) and Type 2 Diabetes Mellitus (T2DM) are chronic conditions that significantly impact public health. Emerging evidence suggests a relationship between IBD and T2DM, with each potentially influencing the risk of the other. Mendelian Randomization (MR) uses genetic variants to infer causal relationships, minimizing confounding and reverse causation biases. This meta-analysis evaluates the bidirectional causal association between IBD and T2DM through MR studies.
Methods: We systematically searched PubMed, Scholar and Scopus for studies evaluating the association between T2DM and IBD [Ulcerative colitis (UC) and Crohn’s disease (CD)] using MR analysis until June 2024. We included studies which used SNP sources T2DKP, GWAS mahajan et al 2018, GERA, UKB, DIAGRAM, and MRICU for T2DM and FinnGen, GWAS liu et al 2015, and IIBDGC for IBD, UC and CD. Random effects models were used for pooled odds ratios (OR). Heterogeneity was assessed using I2 statistics and a leave one-out sensitivity analysis was performed.
Results: In the 4 studies included, 271657 SNPs were studied mostly using european and east Asian ancestries. In Our analysis the pooled odds of inverse variance weighted method showed that T2DM decreases the risk of overall IBD (OR: 0.90, 95%CI - 0.87 0.93, P < 0.01;I2 =0%), while the overall IBD increases the risk of T2DM (OR: 1.01, 95%CI - 1.00 1.02, P= 0.02; I2=50.25%). A leave-one-out sensitivity analysis demonstrated that no single study significantly influenced the overall results. In a subgroup analysis either IBD or UC or CD do not increase the risk of T2DM (p=0.94, p=0.1 and p=0.07 respectively).
Discussion: The results of the bidirectional MR meta-analysis suggest that presence of T2DM decreases the risk of IBD which may be related to the use of anti-diabetic medications. Conversely, the occurrence of IBD increases the risk of T2DM. This association between T2DM and IBD/UC/CD may be related to multiple immune responses and changes in metabolic pathways.
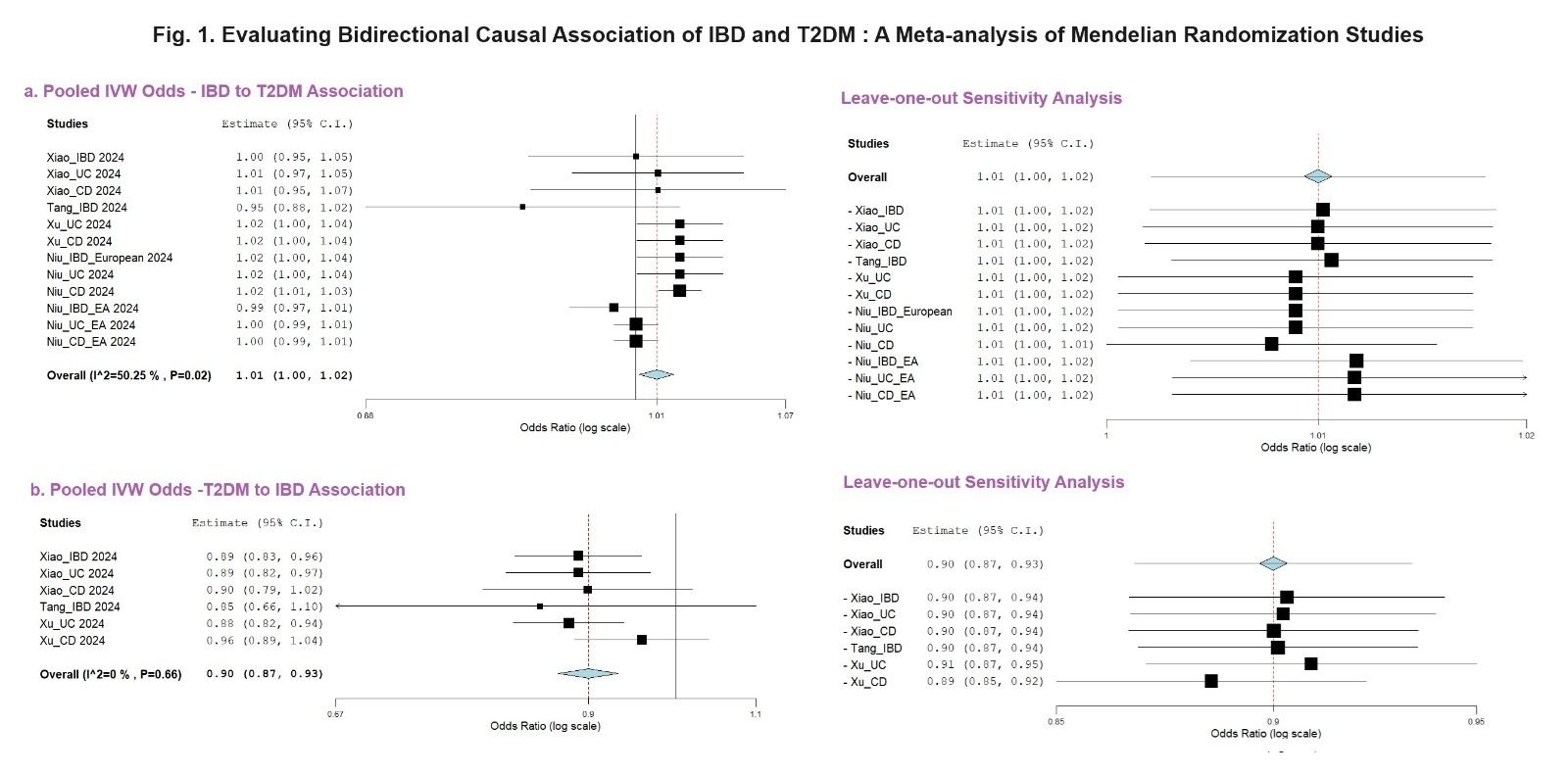
Figure: Forest plot showing bidirectional association between Type 2 diabetes and Inflammatory bowel disease
Disclosures:
Priyatham Gurram indicated no relevant financial relationships.
Shravya Kokkula indicated no relevant financial relationships.
Sricharan Chiluveru indicated no relevant financial relationships.
Moulika kari indicated no relevant financial relationships.
Dayana shre Narayana Swamy indicated no relevant financial relationships.
Akhila Reddy Radhareddy indicated no relevant financial relationships.
Yamini Katamreddy indicated no relevant financial relationships.
George Mathew Mukalil indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Priyatham Gurram, MD1, Shravya K. Kokkula, MBBS2, Sricharan Chiluveru, MBBS3, Moulika kari, MBBS4, Dayana shre Narayana Swamy, MBBS5, Akhila Reddy Radhareddy, MBBS6, Yamini Katamreddy, MD7, George Mathew Mukalil, MD8, Rupak Desai, MBBS9. P0894 - Bidirectional Causal Link Between Type 2 Diabetes Mellitus and Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis of Mendelian Randomization Studies, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
