Sunday Poster Session
Category: IBD
P0929 - Impact of Comorbid Heart Failure Among Hospitalized Patients With Crohn's Disease: A United States Population-Based Cohort Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Karecia Byfield, MBBS
Albert Einstein Medical Center
Philadelphia, PA
Presenting Author(s)
Karecia Byfield, MBBS1, Thanathip Suenghataiphorn, MD2, Phuuwadith Wattanachayakul, MD1, John Malin, DO1, Pojsakorn Danpanichkul, MD3, Chawin Lopimpisuth, MD4, Pakin Lalitnithi, MD5, Natchaya Polpichai, MD6, Sakditad Saowapa, MD3, Bruce Adrian Casipit, MD7, Carlo Gabriel C. Casipit, MD1, Natapat Chaisidhivej, MD8, Mikaela Nikkola Jara-Tantoco, MD1
1Albert Einstein Medical Center, Philadelphia, PA; 2Griffin Hospital, Derby, CT; 3Texas Tech University Health Sciences Center, Lubbock, TX; 4University of Miami Miller School of Medicine, Miami, FL; 5St. Elizabeth’s Medical Center, Boston, MA; 6Weiss Memorial Hospital, Chicago, IL; 7Einstein Medical Center, Philadelphia, PA; 8University of Nebraska Medical Center, Omaha, NE
Introduction: Recent studies have highlighted the adverse outcomes of cardiovascular disorders in individuals with inflammatory bowel disease. However, there is a lack of data regarding the influence of concomitant heart failure (HF), specifically on the outcome among patients primarily hospitalized with Crohn’s disease (CD).
Methods: We analyzed the 2020 U.S. National Inpatient Sample (NIS) to explore the impact of comorbid heart failure (HF) on patients admitted with CD. Participants aged 18 and older were identified using relevant ICD-10 CM codes for CD and other comorbidities. We used multivariable logistic and linear regression analyses to determine the association between comorbid HF and hospital-related outcomes in CD patients.
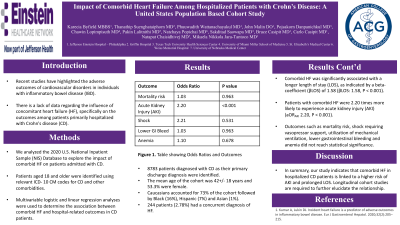
Results: We identified 8,783 patients diagnosed with CD as their primary discharge diagnosis. The mean age of the cohort was 42±18 years, and 53.5% were female. Caucasian accounted for 73%, followed by Black (16%), Mexican American (7%), and Asian (1%). Of the total, 2.78% (244/8,783) had a concurrent diagnosis of HF. Upon adjusting for baseline demographic data and hospital-level confounders, comorbid HF was significantly associated with a longer length of stay (LOS), as indicated by a beta-coefficient (βLOS) of 1.58 (βLOS: 1.58, P < 0.001). Additionally, individuals with comorbid HF were 2.20 times more likely to experience acute kidney injury (AKI) (aORAKI 2.20, P < 0.001). However, other outcomes, including a higher mortality risk (aORmortality1.03, P 0.963), shock requiring vasopressor administration (aORshock 2.21, P 0.531), utilization of mechanical ventilation (aORvent 1.07, P 0.890), the occurrence of lower GI bleeding (aORLGIB 1.03, P 0.963), and anemia (aORanemia 1.10, P 0.678), were observed but did not reach statistical significance.
Discussion: In summary, our study indicates that comorbid HF in hospitalized CD patients is linked to a higher risk of AKI and prolonged LOS. Longitudinal cohort studies are required to further elucidate the relationship.
Disclosures:
Karecia Byfield, MBBS1, Thanathip Suenghataiphorn, MD2, Phuuwadith Wattanachayakul, MD1, John Malin, DO1, Pojsakorn Danpanichkul, MD3, Chawin Lopimpisuth, MD4, Pakin Lalitnithi, MD5, Natchaya Polpichai, MD6, Sakditad Saowapa, MD3, Bruce Adrian Casipit, MD7, Carlo Gabriel C. Casipit, MD1, Natapat Chaisidhivej, MD8, Mikaela Nikkola Jara-Tantoco, MD1. P0929 - Impact of Comorbid Heart Failure Among Hospitalized Patients With Crohn's Disease: A United States Population-Based Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Albert Einstein Medical Center, Philadelphia, PA; 2Griffin Hospital, Derby, CT; 3Texas Tech University Health Sciences Center, Lubbock, TX; 4University of Miami Miller School of Medicine, Miami, FL; 5St. Elizabeth’s Medical Center, Boston, MA; 6Weiss Memorial Hospital, Chicago, IL; 7Einstein Medical Center, Philadelphia, PA; 8University of Nebraska Medical Center, Omaha, NE
Introduction: Recent studies have highlighted the adverse outcomes of cardiovascular disorders in individuals with inflammatory bowel disease. However, there is a lack of data regarding the influence of concomitant heart failure (HF), specifically on the outcome among patients primarily hospitalized with Crohn’s disease (CD).
Methods: We analyzed the 2020 U.S. National Inpatient Sample (NIS) to explore the impact of comorbid heart failure (HF) on patients admitted with CD. Participants aged 18 and older were identified using relevant ICD-10 CM codes for CD and other comorbidities. We used multivariable logistic and linear regression analyses to determine the association between comorbid HF and hospital-related outcomes in CD patients.
Results: We identified 8,783 patients diagnosed with CD as their primary discharge diagnosis. The mean age of the cohort was 42±18 years, and 53.5% were female. Caucasian accounted for 73%, followed by Black (16%), Mexican American (7%), and Asian (1%). Of the total, 2.78% (244/8,783) had a concurrent diagnosis of HF. Upon adjusting for baseline demographic data and hospital-level confounders, comorbid HF was significantly associated with a longer length of stay (LOS), as indicated by a beta-coefficient (βLOS) of 1.58 (βLOS: 1.58, P < 0.001). Additionally, individuals with comorbid HF were 2.20 times more likely to experience acute kidney injury (AKI) (aORAKI 2.20, P < 0.001). However, other outcomes, including a higher mortality risk (aORmortality1.03, P 0.963), shock requiring vasopressor administration (aORshock 2.21, P 0.531), utilization of mechanical ventilation (aORvent 1.07, P 0.890), the occurrence of lower GI bleeding (aORLGIB 1.03, P 0.963), and anemia (aORanemia 1.10, P 0.678), were observed but did not reach statistical significance.
Discussion: In summary, our study indicates that comorbid HF in hospitalized CD patients is linked to a higher risk of AKI and prolonged LOS. Longitudinal cohort studies are required to further elucidate the relationship.
Disclosures:
Karecia Byfield indicated no relevant financial relationships.
Thanathip Suenghataiphorn indicated no relevant financial relationships.
Phuuwadith Wattanachayakul indicated no relevant financial relationships.
John Malin indicated no relevant financial relationships.
Pojsakorn Danpanichkul indicated no relevant financial relationships.
Chawin Lopimpisuth indicated no relevant financial relationships.
Pakin Lalitnithi indicated no relevant financial relationships.
Natchaya Polpichai indicated no relevant financial relationships.
Sakditad Saowapa indicated no relevant financial relationships.
Bruce Adrian Casipit indicated no relevant financial relationships.
Carlo Gabriel Casipit indicated no relevant financial relationships.
Natapat Chaisidhivej indicated no relevant financial relationships.
Mikaela Nikkola Jara-Tantoco indicated no relevant financial relationships.
Karecia Byfield, MBBS1, Thanathip Suenghataiphorn, MD2, Phuuwadith Wattanachayakul, MD1, John Malin, DO1, Pojsakorn Danpanichkul, MD3, Chawin Lopimpisuth, MD4, Pakin Lalitnithi, MD5, Natchaya Polpichai, MD6, Sakditad Saowapa, MD3, Bruce Adrian Casipit, MD7, Carlo Gabriel C. Casipit, MD1, Natapat Chaisidhivej, MD8, Mikaela Nikkola Jara-Tantoco, MD1. P0929 - Impact of Comorbid Heart Failure Among Hospitalized Patients With Crohn's Disease: A United States Population-Based Cohort Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
