Sunday Poster Session
Category: IBD
P0934 - Prevalence and Risk Factors for Ulcerative Colitis Flares After Colonoscopy
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- FK
Fatima Khan, MD
Yale Digestive Diseases
New Haven, CT
Presenting Author(s)
Fatima Khan, MD1, Sunny Chung, MD, MHS1, Bashar Kadhim, MD, MHS2, Prince Ameyaw, MD3, Jonathan Fetene, MD4, Armando Dominguez-Diaz, MD3, Badr Al-Bawardy, MD5, Alexander N. Levy, MD1, Deborah D. Proctor, MD1, Jill Gaidos, MD, FACG1
1Yale Digestive Diseases, New Haven, CT; 2Yale University School of Medicine, New Haven, CT; 3Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 4Yale New Haven Hospital, New Haven, CT; 5King Faisal Specialist Hospital and Research Centre, Riyadh, Ar Riyad, Saudi Arabia
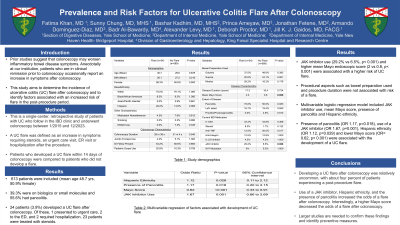
Introduction: Prior studies suggest that colonoscopy may worsen inflammatory bowel disease (IBD) symptoms. Anecdotally at our institution, patients who are in clinical remission prior to colonoscopy occasionally report an increase in symptoms after colonoscopy. This study aims to determine the incidence of ulcerative colitis (UC) flare after colonoscopy and to identify factors associated with an increased risk of flare in the post-procedure period.
Methods: This is a single-center, retrospective study of patients with UC who follow in the IBD clinic and underwent colonoscopy between 1/2015 and 12/2023. A UC flare was defined as an increase in symptoms requiring steroids, an urgent care visit, ER visit or hospitalization after the procedure. Patients who developed a UC flare within 14 days of colonoscopy were compared to patients who did not develop a flare.
Results: We identified 613 patients with UC who underwent colonoscopy during the study period. Overall, mean age was 48.7 years, 50.9% were female, 39.3% were on biologics or small molecules, and 55.6% had pancolitis. A total of 24 patients (3.9%) developed a UC flare after colonoscopy. Of these, 1 presented to urgent care, 2 to the ED, and 2 required hospitalization. Twenty-three patients were treated with steroids. On univariate analysis, JAK inhibitor use (29.2% vs 6.5%, p< 0.001) and higher mean Mayo endoscopic score (2 vs 0.8, p< 0.001) were associated with a higher risk of UC flare [Table 1]. Procedural aspects such as bowel preparation used and procedure duration were not associated with risk of a flare. A multivariable logistic regression model including JAK inhibitor use, mean Mayo score, presence of pancolitis and Hispanic ethnicity showed that presence of pancolitis (p=0.018), use of a JAK inhibitor (p=0.001), Hispanic ethnicity (p=0.029) and lower Mayo score (p< 0.001) were independently associated with the development of a UC flare.
Discussion: Overall, the development of a UC flare after colonoscopy was relatively uncommon, with approximately four percent of patients experiencing a flare post- procedure. Use of a JAK inhibitor, Hispanic ethnicity, lower Mayo score and the presence of pancolitis were independently associated with a higher risk of UC flare after colonoscopy. Larger studies are needed to confirm these findings and identify preventive measures.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Fatima Khan, MD1, Sunny Chung, MD, MHS1, Bashar Kadhim, MD, MHS2, Prince Ameyaw, MD3, Jonathan Fetene, MD4, Armando Dominguez-Diaz, MD3, Badr Al-Bawardy, MD5, Alexander N. Levy, MD1, Deborah D. Proctor, MD1, Jill Gaidos, MD, FACG1. P0934 - Prevalence and Risk Factors for Ulcerative Colitis Flares After Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Yale Digestive Diseases, New Haven, CT; 2Yale University School of Medicine, New Haven, CT; 3Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 4Yale New Haven Hospital, New Haven, CT; 5King Faisal Specialist Hospital and Research Centre, Riyadh, Ar Riyad, Saudi Arabia
Introduction: Prior studies suggest that colonoscopy may worsen inflammatory bowel disease (IBD) symptoms. Anecdotally at our institution, patients who are in clinical remission prior to colonoscopy occasionally report an increase in symptoms after colonoscopy. This study aims to determine the incidence of ulcerative colitis (UC) flare after colonoscopy and to identify factors associated with an increased risk of flare in the post-procedure period.
Methods: This is a single-center, retrospective study of patients with UC who follow in the IBD clinic and underwent colonoscopy between 1/2015 and 12/2023. A UC flare was defined as an increase in symptoms requiring steroids, an urgent care visit, ER visit or hospitalization after the procedure. Patients who developed a UC flare within 14 days of colonoscopy were compared to patients who did not develop a flare.
Results: We identified 613 patients with UC who underwent colonoscopy during the study period. Overall, mean age was 48.7 years, 50.9% were female, 39.3% were on biologics or small molecules, and 55.6% had pancolitis. A total of 24 patients (3.9%) developed a UC flare after colonoscopy. Of these, 1 presented to urgent care, 2 to the ED, and 2 required hospitalization. Twenty-three patients were treated with steroids. On univariate analysis, JAK inhibitor use (29.2% vs 6.5%, p< 0.001) and higher mean Mayo endoscopic score (2 vs 0.8, p< 0.001) were associated with a higher risk of UC flare [Table 1]. Procedural aspects such as bowel preparation used and procedure duration were not associated with risk of a flare. A multivariable logistic regression model including JAK inhibitor use, mean Mayo score, presence of pancolitis and Hispanic ethnicity showed that presence of pancolitis (p=0.018), use of a JAK inhibitor (p=0.001), Hispanic ethnicity (p=0.029) and lower Mayo score (p< 0.001) were independently associated with the development of a UC flare.
Discussion: Overall, the development of a UC flare after colonoscopy was relatively uncommon, with approximately four percent of patients experiencing a flare post- procedure. Use of a JAK inhibitor, Hispanic ethnicity, lower Mayo score and the presence of pancolitis were independently associated with a higher risk of UC flare after colonoscopy. Larger studies are needed to confirm these findings and identify preventive measures.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Fatima Khan indicated no relevant financial relationships.
Sunny Chung indicated no relevant financial relationships.
Bashar Kadhim indicated no relevant financial relationships.
Prince Ameyaw indicated no relevant financial relationships.
Jonathan Fetene indicated no relevant financial relationships.
Armando Dominguez-Diaz indicated no relevant financial relationships.
Badr Al-Bawardy: AbbVie – Consultant, Speakers Bureau. Janssen – Speakers Bureau. Pfizer – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Takeda – Speakers Bureau.
Alexander Levy indicated no relevant financial relationships.
Deborah Proctor indicated no relevant financial relationships.
Jill Gaidos: Abbvie – Advisor or Review Panel Member, Grant/Research Support. Bristol Myers Squibb – Grant/Research Support. Janssen – Grant/Research Support. MRM Health – Consultant. Pfizer – Consultant, Grant/Research Support.
Fatima Khan, MD1, Sunny Chung, MD, MHS1, Bashar Kadhim, MD, MHS2, Prince Ameyaw, MD3, Jonathan Fetene, MD4, Armando Dominguez-Diaz, MD3, Badr Al-Bawardy, MD5, Alexander N. Levy, MD1, Deborah D. Proctor, MD1, Jill Gaidos, MD, FACG1. P0934 - Prevalence and Risk Factors for Ulcerative Colitis Flares After Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
