Sunday Poster Session
Category: IBD
P0936 - Clinical Characteristics and Outcomes of Appendiceal Neoplasms in Inflammatory Bowel Disease: A Case Control Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Siri A. Urquhart, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Siri A. Urquhart, MD, Luis E. Ospina Velasquez, , John B. Kisiel, MD, Nayantara Coelho-Prabhu, MD, FACG
Mayo Clinic, Rochester, MN
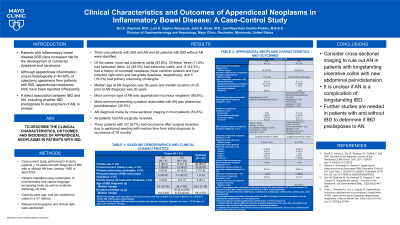
Introduction: Patients with inflammatory bowel disease (IBD), including ulcerative colitis (UC), Crohn’s disease (CD), and indeterminate colitis (IC) face increased risk for the development of colorectal dysplasia and carcinoma. Although appendiceal inflammation occurs histologically in 40-80% of colectomy specimens from patients with IBD, appendiceal neoplasms (AN) have been reported infrequently. A direct association between IBD and AN, including whether IBD predisposes to development of AN, is unclear.
Methods: A case-control study was performed to include patients > 18-years-old with a diagnosis of IBD with or without AN at a single large referral center form January 1992 to April 2023. Patients were identified using a combination of bioinformatics and natural language processing tools, as well as anatomic pathology records. Controls were age- and sex-matched to cases in a 2:1 fashion. Relevant demographic and clinical data were abstracted.
Results: In total 31 patients with IBD and AN and 62 patients with IBD without AN were identified. Of the cases, a majority had UC (83.9%). Of these, three (11.5%) had backwash ileitis, 23 (88.5%) had extensive colitis, 11 (42.3%) had a history of colorectal neoplasia (most common location and type included right colon and low-grade dysplasia, respectively), and 5 (19.2%) had primary sclerosing cholangitis (PSC). Median age at AN diagnosis was 59 years and median duration of UC prior to AN diagnosis was 20 years. The most common type of AN was appendiceal mucinous neoplasm (80.8%). The most common presenting symptom associated with AN was abdominal pain/distension (38.5%). AN diagnosis was made by cross-sectional imaging in a majority of patients (53.8%). All patients had AN surgically resected. Three patients with UC (9.7%) had recurrence after surgical resection due to peritoneal seeding with median time from initial diagnosis to recurrence of 78 months.
Discussion: ANs must be considered in patients with longstanding UC presenting with abdominal pain/distension. Although the incidence and recurrence of AN in patients with IBD is relatively low, further studies to compare AN in patients with and without IBD are needed to determine if IBD predisposes to development of this neoplastic complication.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Siri A. Urquhart, MD, Luis E. Ospina Velasquez, , John B. Kisiel, MD, Nayantara Coelho-Prabhu, MD, FACG. P0936 - Clinical Characteristics and Outcomes of Appendiceal Neoplasms in Inflammatory Bowel Disease: A Case Control Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Patients with inflammatory bowel disease (IBD), including ulcerative colitis (UC), Crohn’s disease (CD), and indeterminate colitis (IC) face increased risk for the development of colorectal dysplasia and carcinoma. Although appendiceal inflammation occurs histologically in 40-80% of colectomy specimens from patients with IBD, appendiceal neoplasms (AN) have been reported infrequently. A direct association between IBD and AN, including whether IBD predisposes to development of AN, is unclear.
Methods: A case-control study was performed to include patients > 18-years-old with a diagnosis of IBD with or without AN at a single large referral center form January 1992 to April 2023. Patients were identified using a combination of bioinformatics and natural language processing tools, as well as anatomic pathology records. Controls were age- and sex-matched to cases in a 2:1 fashion. Relevant demographic and clinical data were abstracted.
Results: In total 31 patients with IBD and AN and 62 patients with IBD without AN were identified. Of the cases, a majority had UC (83.9%). Of these, three (11.5%) had backwash ileitis, 23 (88.5%) had extensive colitis, 11 (42.3%) had a history of colorectal neoplasia (most common location and type included right colon and low-grade dysplasia, respectively), and 5 (19.2%) had primary sclerosing cholangitis (PSC). Median age at AN diagnosis was 59 years and median duration of UC prior to AN diagnosis was 20 years. The most common type of AN was appendiceal mucinous neoplasm (80.8%). The most common presenting symptom associated with AN was abdominal pain/distension (38.5%). AN diagnosis was made by cross-sectional imaging in a majority of patients (53.8%). All patients had AN surgically resected. Three patients with UC (9.7%) had recurrence after surgical resection due to peritoneal seeding with median time from initial diagnosis to recurrence of 78 months.
Discussion: ANs must be considered in patients with longstanding UC presenting with abdominal pain/distension. Although the incidence and recurrence of AN in patients with IBD is relatively low, further studies to compare AN in patients with and without IBD are needed to determine if IBD predisposes to development of this neoplastic complication.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Siri Urquhart indicated no relevant financial relationships.
Luis Ospina Velasquez indicated no relevant financial relationships.
John Kisiel: Exact Sciences – Advisor or Review Panel Member, Advisory Committee/Board Member, Consultant, Grant/Research Support, Intellectual Property/Patents, all paid to Mayo Clinic, Royalties.
Nayantara Coelho-Prabhu: Iterative Health – Advisory Committee/Board Member.
Siri A. Urquhart, MD, Luis E. Ospina Velasquez, , John B. Kisiel, MD, Nayantara Coelho-Prabhu, MD, FACG. P0936 - Clinical Characteristics and Outcomes of Appendiceal Neoplasms in Inflammatory Bowel Disease: A Case Control Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
