Sunday Poster Session
Category: IBD
P0940 - Distinct Demographic and Comorbidity Profiles in Patients with Inflammatory Bowel Disease and Comorbid Celiac Disease: A Comparative Analysis from National Inpatient Sample
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Sajana Poudel, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Sajana Poudel, MD1, Manoj Ghimire, MD2, Ayusha Poudel, MD1, Karun Shrestha, MD2, Kalpana Ghimire, MD2, Prakriti Subedi, MD3, Calvin Ghimire, MD4
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2St. Barnabas Hospital, Bronx, NY; 3St. Barnabas Hospital, New York, NY; 4McLaren Flint Hospital, Flint, MI
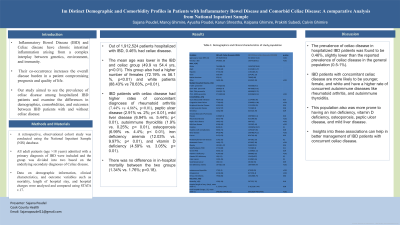
Introduction: Both inflammatory bowel disease (IBD) and celiac disease have chronic intestinal inflammation that arises from the interplay between genetics, environment, and immunity. Their co-occurrence increases the overall disease burden in a patient, compromising prognosis and quality of life. Our study aimed to see the prevalence of celiac disease among hospitalized IBD patients and examine the differences in demographics, comorbidities, and outcomes between IBD patients with and without celiac disease.
Methods: We conducted a retrospective observational study using the National Inpatient Sample (NIS) database from 2016 to 2021. Patients hospitalized with IBD, and more than 18 years of age were identified using the International Classification of Disease-10 codes. The study population was divided into two groups based on the presence or absence of celiac disease. The demographic and clinical characteristics and outcomes of these two groups were compared. Data was analyzed using STATA v.17.
Results: Out of 1,912,524 patients hospitalized with IBD, 0.46% had celiac disease. The mean age was lower in the IBD and celiac group (49.94 years vs 54.3 years; p< 0.01). This group had more females (72.19% vs 56.1%; p< 0.01) and white patients (88.43% vs 78.63%; p< 0.01). IBD patients with celiac disease had higher rates of rheumatoid disease (7.44% vs. 4.86%; p< 0.01), peptic ulcer disease (2.91% vs. 2%; p< 0.01), mild liver disease (6.94% vs. 5.44%; p< 0.01), autoimmune thyroiditis (1.9% vs. 0.25%; p< 0.01), osteoporosis (6.99% vs. 4.4%; p< 0.01), iron deficiency anemia (12.03% vs. 9.97%; p< 0.01), and vitamin D deficiency (4.59% vs. 3.05%; p< 0.01). There was no difference in in-hospital mortality between the two groups (1.34% vs. 1.76%; p=0.18).
Discussion: The prevalence of celiac disease in hospitalized IBD patients was found to be 0.46%, slightly lower than the reported prevalence of celiac disease in the general population (0.5-1%). IBD patients with concomitant celiac disease are more likely to be younger, female, and white and have a higher rate of concurrent autoimmune diseases like rheumatoid arthritis, and autoimmune thyroiditis. This population also was more prone to having an iron deficiency, vitamin D deficiency, osteoporosis, peptic ulcer disease, and mild liver disease. Insights into these associations can help in better management of IBD patients with concurrent celiac disease.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sajana Poudel, MD1, Manoj Ghimire, MD2, Ayusha Poudel, MD1, Karun Shrestha, MD2, Kalpana Ghimire, MD2, Prakriti Subedi, MD3, Calvin Ghimire, MD4. P0940 - Distinct Demographic and Comorbidity Profiles in Patients with Inflammatory Bowel Disease and Comorbid Celiac Disease: A Comparative Analysis from National Inpatient Sample, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2St. Barnabas Hospital, Bronx, NY; 3St. Barnabas Hospital, New York, NY; 4McLaren Flint Hospital, Flint, MI
Introduction: Both inflammatory bowel disease (IBD) and celiac disease have chronic intestinal inflammation that arises from the interplay between genetics, environment, and immunity. Their co-occurrence increases the overall disease burden in a patient, compromising prognosis and quality of life. Our study aimed to see the prevalence of celiac disease among hospitalized IBD patients and examine the differences in demographics, comorbidities, and outcomes between IBD patients with and without celiac disease.
Methods: We conducted a retrospective observational study using the National Inpatient Sample (NIS) database from 2016 to 2021. Patients hospitalized with IBD, and more than 18 years of age were identified using the International Classification of Disease-10 codes. The study population was divided into two groups based on the presence or absence of celiac disease. The demographic and clinical characteristics and outcomes of these two groups were compared. Data was analyzed using STATA v.17.
Results: Out of 1,912,524 patients hospitalized with IBD, 0.46% had celiac disease. The mean age was lower in the IBD and celiac group (49.94 years vs 54.3 years; p< 0.01). This group had more females (72.19% vs 56.1%; p< 0.01) and white patients (88.43% vs 78.63%; p< 0.01). IBD patients with celiac disease had higher rates of rheumatoid disease (7.44% vs. 4.86%; p< 0.01), peptic ulcer disease (2.91% vs. 2%; p< 0.01), mild liver disease (6.94% vs. 5.44%; p< 0.01), autoimmune thyroiditis (1.9% vs. 0.25%; p< 0.01), osteoporosis (6.99% vs. 4.4%; p< 0.01), iron deficiency anemia (12.03% vs. 9.97%; p< 0.01), and vitamin D deficiency (4.59% vs. 3.05%; p< 0.01). There was no difference in in-hospital mortality between the two groups (1.34% vs. 1.76%; p=0.18).
Discussion: The prevalence of celiac disease in hospitalized IBD patients was found to be 0.46%, slightly lower than the reported prevalence of celiac disease in the general population (0.5-1%). IBD patients with concomitant celiac disease are more likely to be younger, female, and white and have a higher rate of concurrent autoimmune diseases like rheumatoid arthritis, and autoimmune thyroiditis. This population also was more prone to having an iron deficiency, vitamin D deficiency, osteoporosis, peptic ulcer disease, and mild liver disease. Insights into these associations can help in better management of IBD patients with concurrent celiac disease.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sajana Poudel indicated no relevant financial relationships.
Manoj Ghimire indicated no relevant financial relationships.
Ayusha Poudel indicated no relevant financial relationships.
Karun Shrestha indicated no relevant financial relationships.
Kalpana Ghimire indicated no relevant financial relationships.
Prakriti Subedi indicated no relevant financial relationships.
Calvin Ghimire indicated no relevant financial relationships.
Sajana Poudel, MD1, Manoj Ghimire, MD2, Ayusha Poudel, MD1, Karun Shrestha, MD2, Kalpana Ghimire, MD2, Prakriti Subedi, MD3, Calvin Ghimire, MD4. P0940 - Distinct Demographic and Comorbidity Profiles in Patients with Inflammatory Bowel Disease and Comorbid Celiac Disease: A Comparative Analysis from National Inpatient Sample, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
