Sunday Poster Session
Category: IBD
P0941 - Assessing the Cardiovascular Risk in Inflammatory Bowel Disease: Insights from Mendelian Randomization Meta-Analysis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E


Ahmad Al Homaid, MD
Nazareth Hospital
Philadelphia, PA
Presenting Author(s)
Ahmad Al Homaid, MD1, Supti Dev Nath, MBBS2, Arankesh Mahadevan, MD3, Sai Gautham Kanagala, MD4, Srikara Gondhi, MBBS5, Nikitha Chellapuram, MD6, Rupak Desai, MBBS7
1Nazareth Hospital, Philadelphia, PA; 2Johns Hopkins University, Baltimore, MD; 3University of Utah Health, Salt Lake City, UT; 4NYC Health + Hospitals/Metropolitan, New York, NY; 5Advocate Illinois Masonic Medical Center, Chicago, IL; 6Centinela Hospital Medical Center, Los Angeles, CA; 7Outcomes Research, Atlanta, GA
Introduction: Observational studies have demonstrated an association between Inflammatory Bowel Disease (IBD) and Cardiovascular Disease (CVD). However, this observed effect is subject to confounding factors and biases. Therefore, the role of IBD in developing CVD remains unclear. Mendelian Randomization (MR) is a method that utilizes genetic variants to study disease causation. Using MR, this meta-analysis aims to explore the causal relationship between IBD and CVD.
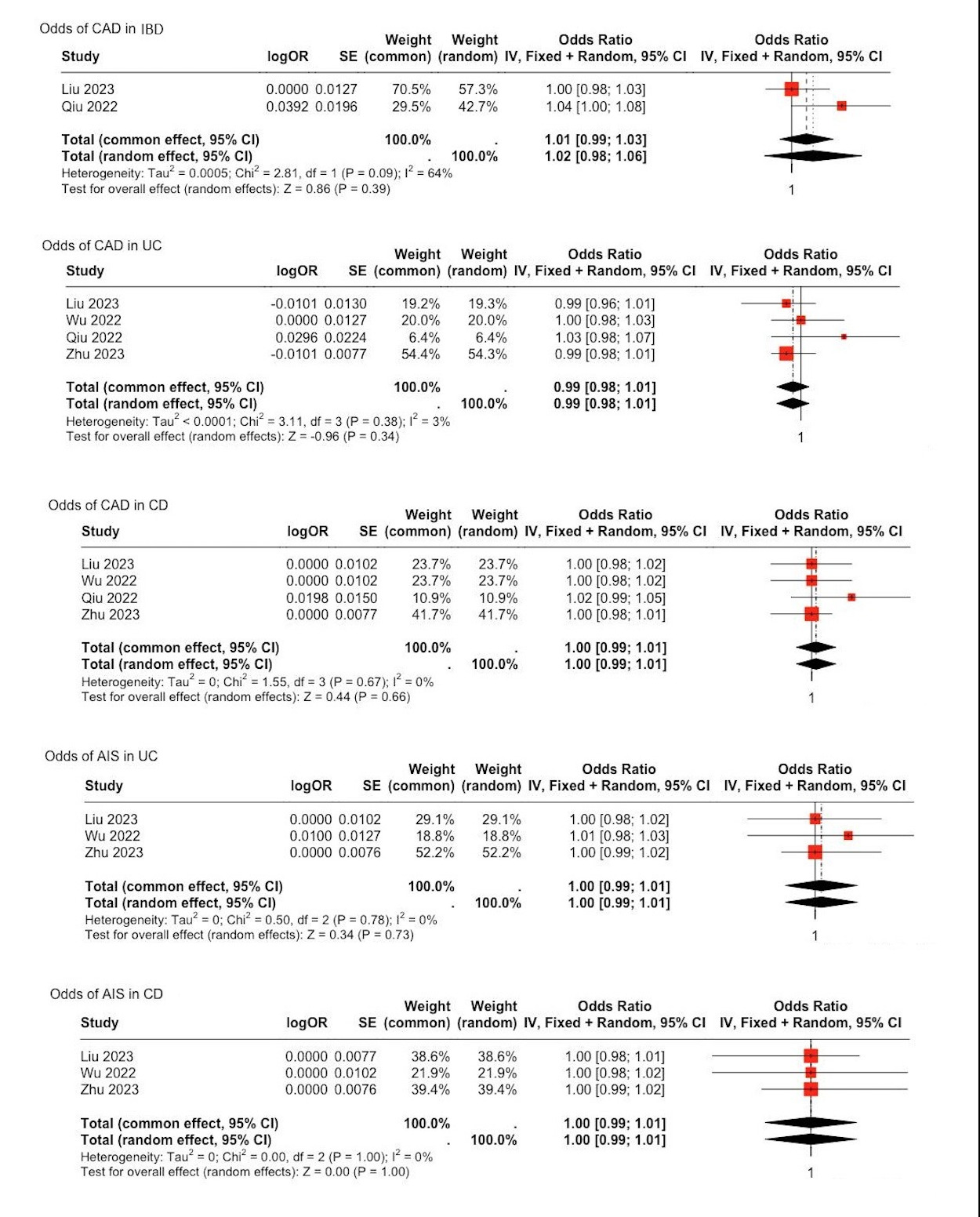
Methods: A comprehensive literature search was conducted in PubMed, EMBASE, and Google Scholar databases up to May 2024 to identify MR studies examining the causal effect of IBD on CVD. Inclusion criteria were MR studies with clearly defined genetic instruments for IBD and outcome measures for CVD, including Coronary Artery Disease (CAD) and Acute Ischemic Stroke (AIS). Data were extracted and pooled using a random-effects meta-analysis model. Heterogeneity was assessed using the I² statistic, tau², and Cochran's Q test.
Results: A total of 4 MR studies were found in our search. The data comprised 36,737 cases of Ulcerative Colitis (UC) and 37,908 cases of Crohn’s Disease (CD). Outcome data included 230,738 cases of CAD and 102,651 cases of AIS. MR analysis revealed no significant association between IBD and CAD [OR 1.01, 95% CI 0.99-1.03]. Further analysis revealed no association between UC and CAD [OR 0.99, 95% CI 0.98-1.01], or between CD and CAD [OR 1.00, 95% CI 0.99-1.01]. Additionally, there was no causal association between UC and AIS [OR 1.00, 95% CI 0.99-1.01], or between CD and AIS [OR 1.00, 95% CI 0.99-1.01]. Except for the relationship between CAD and IBD, heterogeneity remained very low to non-significant.
Discussion: This MR meta-analysis does not support a causal relationship between Inflammatory Bowel Disease and an increased risk of Coronary Artery Disease or Acute Ischemic Stroke. These findings suggest that the previously observed associations may be attributable to confounding factors rather than a direct causal effect. Further research to identify those confounders could enhance our knowledge of the interaction between IBD and CVD.
Disclosures:
Ahmad Al Homaid, MD1, Supti Dev Nath, MBBS2, Arankesh Mahadevan, MD3, Sai Gautham Kanagala, MD4, Srikara Gondhi, MBBS5, Nikitha Chellapuram, MD6, Rupak Desai, MBBS7. P0941 - Assessing the Cardiovascular Risk in Inflammatory Bowel Disease: Insights from Mendelian Randomization Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Nazareth Hospital, Philadelphia, PA; 2Johns Hopkins University, Baltimore, MD; 3University of Utah Health, Salt Lake City, UT; 4NYC Health + Hospitals/Metropolitan, New York, NY; 5Advocate Illinois Masonic Medical Center, Chicago, IL; 6Centinela Hospital Medical Center, Los Angeles, CA; 7Outcomes Research, Atlanta, GA
Introduction: Observational studies have demonstrated an association between Inflammatory Bowel Disease (IBD) and Cardiovascular Disease (CVD). However, this observed effect is subject to confounding factors and biases. Therefore, the role of IBD in developing CVD remains unclear. Mendelian Randomization (MR) is a method that utilizes genetic variants to study disease causation. Using MR, this meta-analysis aims to explore the causal relationship between IBD and CVD.
Methods: A comprehensive literature search was conducted in PubMed, EMBASE, and Google Scholar databases up to May 2024 to identify MR studies examining the causal effect of IBD on CVD. Inclusion criteria were MR studies with clearly defined genetic instruments for IBD and outcome measures for CVD, including Coronary Artery Disease (CAD) and Acute Ischemic Stroke (AIS). Data were extracted and pooled using a random-effects meta-analysis model. Heterogeneity was assessed using the I² statistic, tau², and Cochran's Q test.
Results: A total of 4 MR studies were found in our search. The data comprised 36,737 cases of Ulcerative Colitis (UC) and 37,908 cases of Crohn’s Disease (CD). Outcome data included 230,738 cases of CAD and 102,651 cases of AIS. MR analysis revealed no significant association between IBD and CAD [OR 1.01, 95% CI 0.99-1.03]. Further analysis revealed no association between UC and CAD [OR 0.99, 95% CI 0.98-1.01], or between CD and CAD [OR 1.00, 95% CI 0.99-1.01]. Additionally, there was no causal association between UC and AIS [OR 1.00, 95% CI 0.99-1.01], or between CD and AIS [OR 1.00, 95% CI 0.99-1.01]. Except for the relationship between CAD and IBD, heterogeneity remained very low to non-significant.
Discussion: This MR meta-analysis does not support a causal relationship between Inflammatory Bowel Disease and an increased risk of Coronary Artery Disease or Acute Ischemic Stroke. These findings suggest that the previously observed associations may be attributable to confounding factors rather than a direct causal effect. Further research to identify those confounders could enhance our knowledge of the interaction between IBD and CVD.
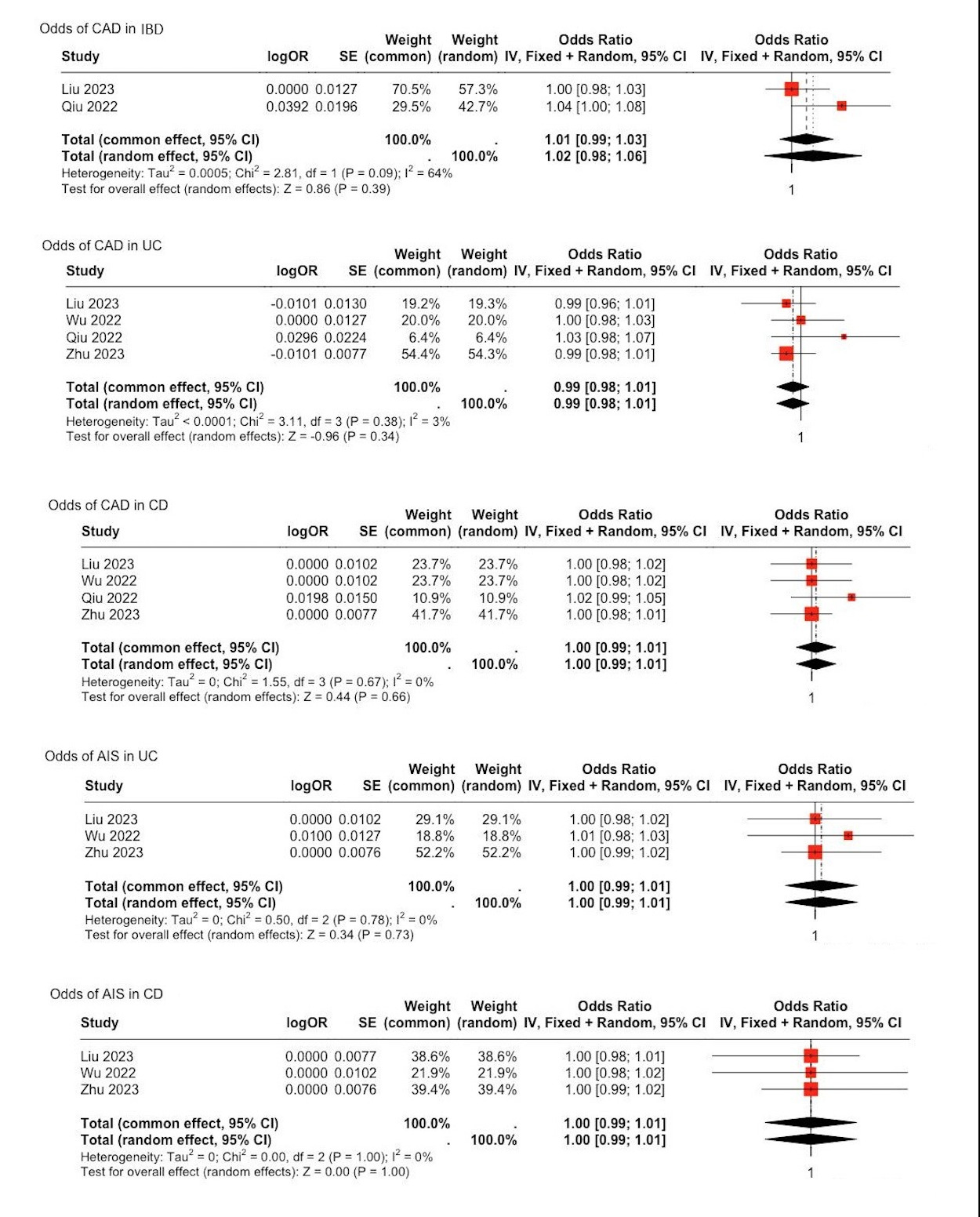
Figure: Fig.1. Evaluation of Causative Role of IBD in CAD and AIS: a Meta-analysis of Mendelian Randomization Studies
Disclosures:
Ahmad Al Homaid indicated no relevant financial relationships.
Supti Dev Nath indicated no relevant financial relationships.
Arankesh Mahadevan indicated no relevant financial relationships.
Sai Gautham Kanagala indicated no relevant financial relationships.
Srikara Gondhi indicated no relevant financial relationships.
Nikitha Chellapuram indicated no relevant financial relationships.
Rupak Desai indicated no relevant financial relationships.
Ahmad Al Homaid, MD1, Supti Dev Nath, MBBS2, Arankesh Mahadevan, MD3, Sai Gautham Kanagala, MD4, Srikara Gondhi, MBBS5, Nikitha Chellapuram, MD6, Rupak Desai, MBBS7. P0941 - Assessing the Cardiovascular Risk in Inflammatory Bowel Disease: Insights from Mendelian Randomization Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
