Sunday Poster Session
Category: IBD
P0972 - The Missing Link: Crohn’s Disease and Concomitant Mucous Membrane Pemphigoid
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Marisa-Nicole Zayat, MD
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Micah Vander Griend, MPH1, Marisa-Nicole Zayat, MD1, Diala Merheb, MD1, Mahmoud Mahdi, MD1, Hana Razek, MD2, Estephan Zayat, MD3
1University of Kansas School of Medicine, Wichita, KS; 2Heartland Pathology, Wichita, KS; 3Kansas Gastroenterology and Endoscopy, LLC, Wichita, KS
Introduction: Crohn’s disease is an inflammatory bowel disease that can present anywhere along the GI tract. Bullous pemphigoid and mucous membrane pemphigoid are uncommon autoimmune subepithelial blistering diseases that most frequently arise in older adults and are characterized by cutaneous bullae and erosive mucosal lesions. An association with Crohn’s disease has not been established.
Case Description/Methods: An 80-year-old man with a past medical history significant for diverticulosis and atrial fibrillation presented to the ED with new-onset hematochezia. His home aspirin and rivaroxaban were held. His hemoglobin on admission was 9.7 g/dL. CT revealed thickening of the sigmoid colon and rectum, suspicious of an inflammatory process. A partial colonoscopy performed by the on-call surgeon found diffuse colitis with ulceration. Biopsies were not obtained.
Upon a more thorough review, it was noted that he had previously seen an oral surgeon who found oral blisters suspicious for pemphigus vulgaris for which he was referred to dermatology. During that time, the patient also began to experience cutaneous blistering. A punch biopsy was consistent with mucous membrane pemphigoid. Serum studies noted elevated BP180 antibodies. Due to the patient's history of mucous membrane pemphigoid, the surgery team suspected that his endoscopic findings may correlate. Gastroenterology was consulted.
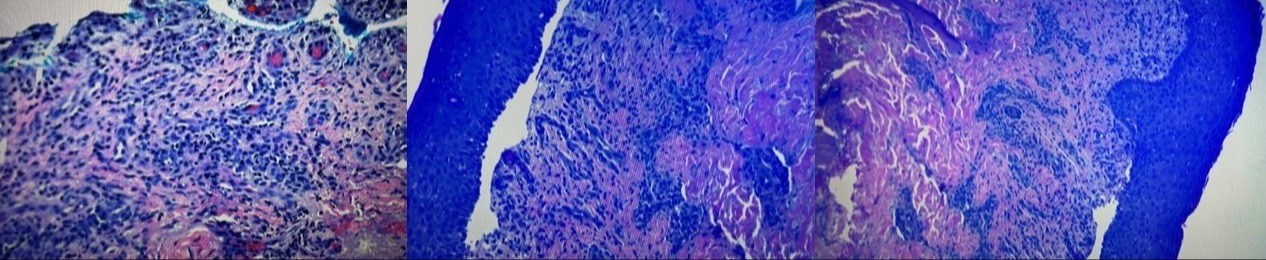
Repeat colonoscopy found multiple skip areas of serpiginous, punched-out, and superficial ulcers throughout the colon concerning for Crohn's disease. Pathology reported collagenous colitis with patchy mild active colitis, areas of ulceration, neuronal hyperplasia, lymphocytic infiltrate, and minimal chronicity. The biopsy was negative for dysplasia or granulomas. These findings are more consistent with Crohn’s disease given the endoscopic correlate. Capsule study was normal.
Empiric mesalamine and prednisone were initiated, with symptom resolution. He did not have bleeding with the reintroduction of anticoagulation.
Discussion: We present a rare co-occurrence of mucous membrane pemphigoid and Crohn's disease. As of 2012, only 48 cases of subepidermal autoimmune blistering diseases and IBD had been reported in the literature, eight of which were bullous pemphigoid. To our knowledge, this is the first reported case of mucous membrane pemphigoid and Crohn’s disease. Similar to mucous membrane pemphigoid, the pathogenesis of Crohn's disease is thought to be related to IL23 and TH17 dysregulation, making an association plausible.
Disclosures:
Micah Vander Griend, MPH1, Marisa-Nicole Zayat, MD1, Diala Merheb, MD1, Mahmoud Mahdi, MD1, Hana Razek, MD2, Estephan Zayat, MD3. P0972 - The Missing Link: Crohn’s Disease and Concomitant Mucous Membrane Pemphigoid, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kansas School of Medicine, Wichita, KS; 2Heartland Pathology, Wichita, KS; 3Kansas Gastroenterology and Endoscopy, LLC, Wichita, KS
Introduction: Crohn’s disease is an inflammatory bowel disease that can present anywhere along the GI tract. Bullous pemphigoid and mucous membrane pemphigoid are uncommon autoimmune subepithelial blistering diseases that most frequently arise in older adults and are characterized by cutaneous bullae and erosive mucosal lesions. An association with Crohn’s disease has not been established.
Case Description/Methods: An 80-year-old man with a past medical history significant for diverticulosis and atrial fibrillation presented to the ED with new-onset hematochezia. His home aspirin and rivaroxaban were held. His hemoglobin on admission was 9.7 g/dL. CT revealed thickening of the sigmoid colon and rectum, suspicious of an inflammatory process. A partial colonoscopy performed by the on-call surgeon found diffuse colitis with ulceration. Biopsies were not obtained.
Upon a more thorough review, it was noted that he had previously seen an oral surgeon who found oral blisters suspicious for pemphigus vulgaris for which he was referred to dermatology. During that time, the patient also began to experience cutaneous blistering. A punch biopsy was consistent with mucous membrane pemphigoid. Serum studies noted elevated BP180 antibodies. Due to the patient's history of mucous membrane pemphigoid, the surgery team suspected that his endoscopic findings may correlate. Gastroenterology was consulted.
Repeat colonoscopy found multiple skip areas of serpiginous, punched-out, and superficial ulcers throughout the colon concerning for Crohn's disease. Pathology reported collagenous colitis with patchy mild active colitis, areas of ulceration, neuronal hyperplasia, lymphocytic infiltrate, and minimal chronicity. The biopsy was negative for dysplasia or granulomas. These findings are more consistent with Crohn’s disease given the endoscopic correlate. Capsule study was normal.
Empiric mesalamine and prednisone were initiated, with symptom resolution. He did not have bleeding with the reintroduction of anticoagulation.
Discussion: We present a rare co-occurrence of mucous membrane pemphigoid and Crohn's disease. As of 2012, only 48 cases of subepidermal autoimmune blistering diseases and IBD had been reported in the literature, eight of which were bullous pemphigoid. To our knowledge, this is the first reported case of mucous membrane pemphigoid and Crohn’s disease. Similar to mucous membrane pemphigoid, the pathogenesis of Crohn's disease is thought to be related to IL23 and TH17 dysregulation, making an association plausible.
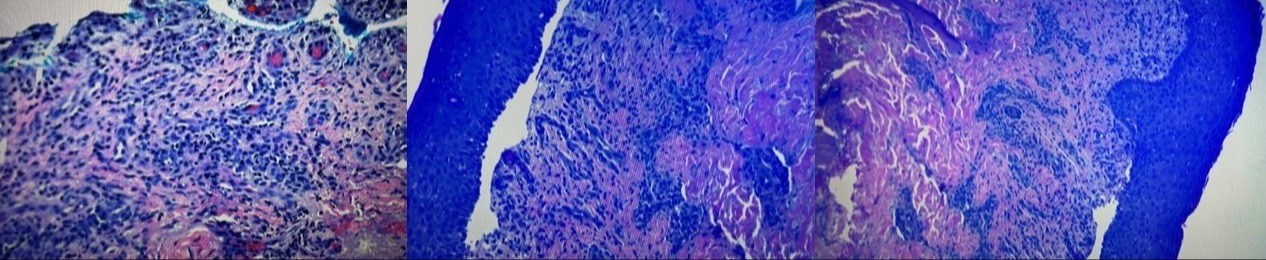
Figure: Figures 1-3. Biopsies depict collagenous colitis with patchy mild active colitis, areas of ulceration, neuronal hyperplasia, lymphocytic infiltrate, and minimal chronicity that were negative for dysplasia or granulomas.
Disclosures:
Micah Vander Griend indicated no relevant financial relationships.
Marisa-Nicole Zayat indicated no relevant financial relationships.
Diala Merheb indicated no relevant financial relationships.
Mahmoud Mahdi indicated no relevant financial relationships.
Hana Razek indicated no relevant financial relationships.
Estephan Zayat indicated no relevant financial relationships.
Micah Vander Griend, MPH1, Marisa-Nicole Zayat, MD1, Diala Merheb, MD1, Mahmoud Mahdi, MD1, Hana Razek, MD2, Estephan Zayat, MD3. P0972 - The Missing Link: Crohn’s Disease and Concomitant Mucous Membrane Pemphigoid, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
