Sunday Poster Session
Category: IBD
P0981 - Hemorrhagic Stroke Secondary to Inflammatory Bowel Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

John Paul Braun, BS
Creighton University School of Medicine
Omaha, NE
Presenting Author(s)
Rees Checketts, DO1, Bridget Hickey, BS1, John Paul Braun, BS1, Robert W. Plambeck, MD2
1Creighton University School of Medicine, Omaha, NE; 2CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Hypercoagulability is a rare complication of ulcerative colitis (UC) with potential for significant morbidity and mortality, especially in the case of embolic cerebrovascular attacks (CVA). This patient had well-controlled UC and yet developed a devastating CVA requiring neurosurgical and intensive care interventions.
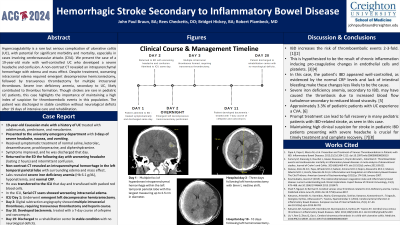
Case Description/Methods: A 19-year-old male with a history of UC, treated with adalimumab, prednisone, and mesalazine, presented to the ED with 3 days of a severe headache, nausea, and vomiting. He received a normal saline bolus, ketorolac, dexamethasone, prochlorperazine, and diphenhydramine, with symptom relief and was discharged. The next day, he returned with a worsening 2 hour long headache and intermittent confusion. A non-contrast CT showed an intraparenchymal hemorrhage in the left temporal parietal lobe with surrounding edema and mass effect. Labs revealed severe iron deficiency anemia, hyponatremia, and normal CRP.
In the ICU he was transfused packed red blood cells. Serial CT scans showed worsening intracranial edema, leading to an emergent left decompressive hemicraniectomy. On day 2, digital subtraction angiography revealed multiple intracranial thromboses, necessitating a transvenous thrombectomy. Heparin infusion was then initiated. On day 10, he developed bacteremia responsive to a 7-day course of cefepime and vancomycin. He was discharged to a rehabilitation center on day 19 in stable condition with no neurological deficits.
Discussion: Inflammatory bowel disease (IBD) increases the risk for thromboembolic events 2-3 fold. Chronic inflammation associated with IBD is a significant risk factor, as it induces pro-coagulative changes in endothelial cells and platelets, among other effects. Paradoxically, this patient’s IBD appeared well-controlled, indicated by a normal CRP and a lack of intestinal bleeding. Instead, severe iron deficiency anemia, secondary to IBD, likely induced thrombosis due to resultant turbulent blood flow.
Strokes are a rare complication of IBD; approximately 3.3% of pediatric patients with UC will experience a cerebrovascular event. In cases of sinus venous thrombosis, the most common presenting symptom is a persistent headache, seen in this case. With prompt treatment, many pediatric patients can recover fully. Maintaining a high clinical suspicion for stroke in pediatric IBD patients is crucial to ensure timely treatment.
Disclosures:
Rees Checketts, DO1, Bridget Hickey, BS1, John Paul Braun, BS1, Robert W. Plambeck, MD2. P0981 - Hemorrhagic Stroke Secondary to Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Creighton University School of Medicine, Omaha, NE; 2CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Hypercoagulability is a rare complication of ulcerative colitis (UC) with potential for significant morbidity and mortality, especially in the case of embolic cerebrovascular attacks (CVA). This patient had well-controlled UC and yet developed a devastating CVA requiring neurosurgical and intensive care interventions.
Case Description/Methods: A 19-year-old male with a history of UC, treated with adalimumab, prednisone, and mesalazine, presented to the ED with 3 days of a severe headache, nausea, and vomiting. He received a normal saline bolus, ketorolac, dexamethasone, prochlorperazine, and diphenhydramine, with symptom relief and was discharged. The next day, he returned with a worsening 2 hour long headache and intermittent confusion. A non-contrast CT showed an intraparenchymal hemorrhage in the left temporal parietal lobe with surrounding edema and mass effect. Labs revealed severe iron deficiency anemia, hyponatremia, and normal CRP.
In the ICU he was transfused packed red blood cells. Serial CT scans showed worsening intracranial edema, leading to an emergent left decompressive hemicraniectomy. On day 2, digital subtraction angiography revealed multiple intracranial thromboses, necessitating a transvenous thrombectomy. Heparin infusion was then initiated. On day 10, he developed bacteremia responsive to a 7-day course of cefepime and vancomycin. He was discharged to a rehabilitation center on day 19 in stable condition with no neurological deficits.
Discussion: Inflammatory bowel disease (IBD) increases the risk for thromboembolic events 2-3 fold. Chronic inflammation associated with IBD is a significant risk factor, as it induces pro-coagulative changes in endothelial cells and platelets, among other effects. Paradoxically, this patient’s IBD appeared well-controlled, indicated by a normal CRP and a lack of intestinal bleeding. Instead, severe iron deficiency anemia, secondary to IBD, likely induced thrombosis due to resultant turbulent blood flow.
Strokes are a rare complication of IBD; approximately 3.3% of pediatric patients with UC will experience a cerebrovascular event. In cases of sinus venous thrombosis, the most common presenting symptom is a persistent headache, seen in this case. With prompt treatment, many pediatric patients can recover fully. Maintaining a high clinical suspicion for stroke in pediatric IBD patients is crucial to ensure timely treatment.
Disclosures:
Rees Checketts indicated no relevant financial relationships.
Bridget Hickey indicated no relevant financial relationships.
John Paul Braun indicated no relevant financial relationships.
Robert Plambeck indicated no relevant financial relationships.
Rees Checketts, DO1, Bridget Hickey, BS1, John Paul Braun, BS1, Robert W. Plambeck, MD2. P0981 - Hemorrhagic Stroke Secondary to Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
