Sunday Poster Session
Category: IBD
P0983 - Atypical Presentations of Immune Checkpoint Inhibitor Colitis on 18-FDG PET/CT: A Case Series
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Kei Takigawa, MD
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Kei Takigawa, MD1, Malek Shatila, MD2, Andres Rivera, MD1, Nitish Mittal, MD3, Abdullah S. Aleem, MD4, Sean Ngo, BS3, Eric Lu, 5, Deanna Wu, 6, Anusha Thomas, MD2, Gabriel Sperling, MD7, Sidra Naz, MD, MPH8, Yinghong Wang, MD, PhD8
1Baylor College of Medicine, Houston, TX; 2The University of Texas MD Anderson Cancer Center, Houston, TX; 3University of Texas Health, McGovern Medical School, Houston, TX; 4University of Texas at Houston, Houston, TX; 5Texas A&M, Bryan, TX; 6Washington University, St. Louis, MO; 7University of Texas Medical Branch, Galveston, TX; 8University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: Immune Checkpoint Inhibitor (ICI) colitis is an immune related adverse event that is commonly associated with therapy of PD-1/PD-L1 inhibitors, CTLA-4 inhibitors or a combination of both.1 Typical presentation of ICI colitis include 1) clinical symptoms of diarrhea, rectal bleeding, mucus, and abdominal pain; 2) endoscopic inflammation; 3) histologic inflammation; and 4) imaging evidence of colitis on FDG PET/CT. This case series aims to highlight atypical cases of ICI colitis to enhance clinical awareness.
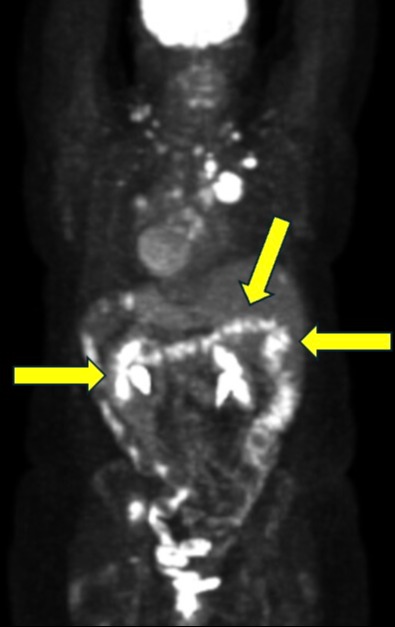
Case Description/Methods: Case 1: A 45-year-old female presented with adenocarcinoma of the lung and was started on combination nivolumab/ipilimumab two months following diagnosis. Weeks following treatment initiation, she experienced watery, non-bloody diarrhea with positive stool lactoferrin and negative stool calprotectin. Colonoscopy revealed grossly normal ileum and colon, however, pathology report showed lymphocytic colitis throughout. PET/CT for staging around the same time showed increased metabolic activity throughout the colon, consistent with symptoms, but not with endoscopy findings.
Case 2: A 54-year-old female with metastatic infiltrating ductal carcinoma of the left breast (ER/PR negative, HER-2 neu 2+) grade 3 with lymphovascular invasion. Following initial treatments with lumpectomy, paclitaxel, trastuzumab, and pertuzumab, patient was switched to nivolumab with PI3K inhibitor due to skin metastasis. After 4 cycles, she developed grade 3 diarrhea with gross endoscopic and histologic inflammation consistent with ICI colitis. Symptoms resolved with IV steroid with subsequent taper. PET/CT for staging prior to and after the colitis episode did not reveal increased uptake in the colon.
Discussion: The cases demonstrate two vastly different PET/CT findings in the setting of ICI colitis. The first case demonstrates positive update on PET/CT despite the colon appearing grossly normal on scope. The second case highlights negative PET/CT despite clinical, endoscopic, and histologic evidence of ICI colitis. These two cases support the need for using multiple diagnostic tools to predict and diagnose ICI colitis.
Conclusion:
Awareness of the atypical presentations of ICI colitis along with variable findings on PET/CT can lead to comprehensive evaluation and potentially improve patient outcomes. Clinicians should continue to use a multifaceted approach in diagnosing ICI colitis and use FDG PET/CT findings judiciously.
Disclosures:
Kei Takigawa, MD1, Malek Shatila, MD2, Andres Rivera, MD1, Nitish Mittal, MD3, Abdullah S. Aleem, MD4, Sean Ngo, BS3, Eric Lu, 5, Deanna Wu, 6, Anusha Thomas, MD2, Gabriel Sperling, MD7, Sidra Naz, MD, MPH8, Yinghong Wang, MD, PhD8. P0983 - Atypical Presentations of Immune Checkpoint Inhibitor Colitis on 18-FDG PET/CT: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Baylor College of Medicine, Houston, TX; 2The University of Texas MD Anderson Cancer Center, Houston, TX; 3University of Texas Health, McGovern Medical School, Houston, TX; 4University of Texas at Houston, Houston, TX; 5Texas A&M, Bryan, TX; 6Washington University, St. Louis, MO; 7University of Texas Medical Branch, Galveston, TX; 8University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: Immune Checkpoint Inhibitor (ICI) colitis is an immune related adverse event that is commonly associated with therapy of PD-1/PD-L1 inhibitors, CTLA-4 inhibitors or a combination of both.1 Typical presentation of ICI colitis include 1) clinical symptoms of diarrhea, rectal bleeding, mucus, and abdominal pain; 2) endoscopic inflammation; 3) histologic inflammation; and 4) imaging evidence of colitis on FDG PET/CT. This case series aims to highlight atypical cases of ICI colitis to enhance clinical awareness.
Case Description/Methods: Case 1: A 45-year-old female presented with adenocarcinoma of the lung and was started on combination nivolumab/ipilimumab two months following diagnosis. Weeks following treatment initiation, she experienced watery, non-bloody diarrhea with positive stool lactoferrin and negative stool calprotectin. Colonoscopy revealed grossly normal ileum and colon, however, pathology report showed lymphocytic colitis throughout. PET/CT for staging around the same time showed increased metabolic activity throughout the colon, consistent with symptoms, but not with endoscopy findings.
Case 2: A 54-year-old female with metastatic infiltrating ductal carcinoma of the left breast (ER/PR negative, HER-2 neu 2+) grade 3 with lymphovascular invasion. Following initial treatments with lumpectomy, paclitaxel, trastuzumab, and pertuzumab, patient was switched to nivolumab with PI3K inhibitor due to skin metastasis. After 4 cycles, she developed grade 3 diarrhea with gross endoscopic and histologic inflammation consistent with ICI colitis. Symptoms resolved with IV steroid with subsequent taper. PET/CT for staging prior to and after the colitis episode did not reveal increased uptake in the colon.
Discussion: The cases demonstrate two vastly different PET/CT findings in the setting of ICI colitis. The first case demonstrates positive update on PET/CT despite the colon appearing grossly normal on scope. The second case highlights negative PET/CT despite clinical, endoscopic, and histologic evidence of ICI colitis. These two cases support the need for using multiple diagnostic tools to predict and diagnose ICI colitis.
Conclusion:
Awareness of the atypical presentations of ICI colitis along with variable findings on PET/CT can lead to comprehensive evaluation and potentially improve patient outcomes. Clinicians should continue to use a multifaceted approach in diagnosing ICI colitis and use FDG PET/CT findings judiciously.
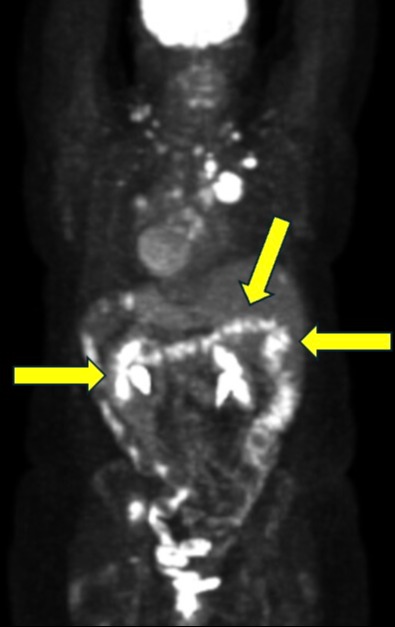
Figure: Figure 1. Increased uptake seen diffusely throughout colon in our patient case #1.
Disclosures:
Kei Takigawa indicated no relevant financial relationships.
Malek Shatila indicated no relevant financial relationships.
Andres Rivera indicated no relevant financial relationships.
Nitish Mittal indicated no relevant financial relationships.
Abdullah Aleem indicated no relevant financial relationships.
Sean Ngo indicated no relevant financial relationships.
Eric Lu indicated no relevant financial relationships.
Deanna Wu indicated no relevant financial relationships.
Anusha Thomas indicated no relevant financial relationships.
Gabriel Sperling indicated no relevant financial relationships.
Sidra Naz indicated no relevant financial relationships.
Yinghong Wang: AzurRx – Consultant. Ilyapharma – Consultant. IOTA – Consultant. Sorriso – Consultant. Tillotts – Consultant.
Kei Takigawa, MD1, Malek Shatila, MD2, Andres Rivera, MD1, Nitish Mittal, MD3, Abdullah S. Aleem, MD4, Sean Ngo, BS3, Eric Lu, 5, Deanna Wu, 6, Anusha Thomas, MD2, Gabriel Sperling, MD7, Sidra Naz, MD, MPH8, Yinghong Wang, MD, PhD8. P0983 - Atypical Presentations of Immune Checkpoint Inhibitor Colitis on 18-FDG PET/CT: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
