Sunday Poster Session
Category: IBD
P1010 - Ustekinumab-Induced Vasculitis in a Patient With Crohn’s Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Siri A. Urquhart, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Luis E. Ospina Velasquez, , Siri A. Urquhart, MD, Konstantinos Papadakis, MD
Mayo Clinic, Rochester, MN
Introduction: Immunoglobulin A (IgA) vasculitis is a small vessel vasculitis characterized by the presence of IgA1 deposits within the vessels. Clinical manifestations may include arthralgias, palpable purpura distributed in the lower extremities, upper extremities, and trunk, as well as renal disease. IgA vasculitis has been reported to be associated with chronic infections, autoimmune disorders, and medications.
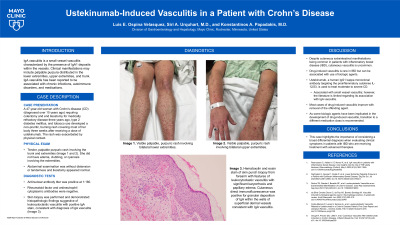
Case Description/Methods: A 47-year-old woman with a longstanding history of Crohn’s disease (CD) requiring colectomy and end ileostomy for medically refractory disease three years ago, type 2 diabetes mellitus, and tobacco use, developed a non-pruritic, burning rash covering a majority of her body three weeks after receiving a dose of ustekinumab. The rash was exacerbated by physical contact. Physical exam was notable for a tender, palpable purpuric rash involving the trunk and extremities (Figure 1A and 1B). She did not have edema, clubbing, or cyanosis involving the extremities. Abdominal examination was without distension or tenderness and ileostomy appeared normal. Antinuclear antibody titer was positive at 1:160. Rheumatoid factor and antineutrophil cytoplasmic antibodies were negative. Skin biopsy demonstrated histopathologic findings suggestive of leukocytoclastic vasculitis with positive IgA stain, consistent with a diagnosis of IgA vasculitis (Figure 1C).
Discussion: Despite cutaneous extraintestinal manifestations being common in patients with inflammatory bowel disease (IBD), cutaneous vasculitis is uncommon. Drug-induced vasculitis is rare in IBD but can be associated with use of biologic agents. Ustekinumab, a human IgG1 kappa monoclonal antibody targeting the proinflammatory cytokines IL-12/23, is used to treat moderate to severe CD. Ustekinumab has been associated with small vessel vasculitis; however, the literature is limited regarding its association with IgA vasculitis. Most cases of drug-induced vasculitis improve with removal of the offending agent. As some biologic agents have been implicated in the development of drug-induced vasculitis, transition to a different medication class is recommended. This case highlights the importance of considering a broad differential diagnosis when evaluating clinical symptoms in patients with IBD who are receiving treatment with advanced therapies.

Disclosures:
Luis E. Ospina Velasquez, , Siri A. Urquhart, MD, Konstantinos Papadakis, MD. P1010 - Ustekinumab-Induced Vasculitis in a Patient With Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Immunoglobulin A (IgA) vasculitis is a small vessel vasculitis characterized by the presence of IgA1 deposits within the vessels. Clinical manifestations may include arthralgias, palpable purpura distributed in the lower extremities, upper extremities, and trunk, as well as renal disease. IgA vasculitis has been reported to be associated with chronic infections, autoimmune disorders, and medications.
Case Description/Methods: A 47-year-old woman with a longstanding history of Crohn’s disease (CD) requiring colectomy and end ileostomy for medically refractory disease three years ago, type 2 diabetes mellitus, and tobacco use, developed a non-pruritic, burning rash covering a majority of her body three weeks after receiving a dose of ustekinumab. The rash was exacerbated by physical contact. Physical exam was notable for a tender, palpable purpuric rash involving the trunk and extremities (Figure 1A and 1B). She did not have edema, clubbing, or cyanosis involving the extremities. Abdominal examination was without distension or tenderness and ileostomy appeared normal. Antinuclear antibody titer was positive at 1:160. Rheumatoid factor and antineutrophil cytoplasmic antibodies were negative. Skin biopsy demonstrated histopathologic findings suggestive of leukocytoclastic vasculitis with positive IgA stain, consistent with a diagnosis of IgA vasculitis (Figure 1C).
Discussion: Despite cutaneous extraintestinal manifestations being common in patients with inflammatory bowel disease (IBD), cutaneous vasculitis is uncommon. Drug-induced vasculitis is rare in IBD but can be associated with use of biologic agents. Ustekinumab, a human IgG1 kappa monoclonal antibody targeting the proinflammatory cytokines IL-12/23, is used to treat moderate to severe CD. Ustekinumab has been associated with small vessel vasculitis; however, the literature is limited regarding its association with IgA vasculitis. Most cases of drug-induced vasculitis improve with removal of the offending agent. As some biologic agents have been implicated in the development of drug-induced vasculitis, transition to a different medication class is recommended. This case highlights the importance of considering a broad differential diagnosis when evaluating clinical symptoms in patients with IBD who are receiving treatment with advanced therapies.

Figure: Figure 1. Visible palpable, purpuric rash involving the bilateral lower (A) and upper (B) extremities. Hematoxylin and eosin stain of skin punch biopsy from forearm with features of leukocytoclastic vasculitis with significant karyorrhexis and papillary edema (C).
Disclosures:
Luis Ospina Velasquez indicated no relevant financial relationships.
Siri Urquhart indicated no relevant financial relationships.
Konstantinos Papadakis: Amgen – Stock-publicly held company(excluding mutual/index funds). Johnson and Johnson – Stock-publicly held company(excluding mutual/index funds). Medtronic – Stock-publicly held company(excluding mutual/index funds).
Luis E. Ospina Velasquez, , Siri A. Urquhart, MD, Konstantinos Papadakis, MD. P1010 - Ustekinumab-Induced Vasculitis in a Patient With Crohn’s Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
