Sunday Poster Session
Category: IBD
P1013 - Ixekizumab-Induced Inflammatory Bowel Disease Catastrophe in the Last Frontier
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- TS
Taylor L. Spiewak
Advocate Christ Medical Center
Oak Lawn, IL
Presenting Author(s)
Taylor L. Spiewak, 1, Ted A. Spiewak, DO2
1Advocate Christ Medical Center, Oak Lawn, IL; 2United States Air Force, Anchorage, AK
Introduction: Patients with psoriatic arthritis have been shown to have a 1-4-fold increased risk, compared to the general population, of developing inflammatory bowel disease (IBD). Ixekizumab (IXE) is one of four monoclonal antibodies targeting interleukin-17 or its receptor, widely used for the treatment of several immune-mediated inflammatory conditions. Despite being reported as rare (< 1%) in clinical trials, cases of new onset and exacerbation of IBD continue to be reported in real-world settings. We report a challenging case with several important learning points of de novo development of severe, complicated Crohn’s disease in a patient on IXE.
Case Description/Methods: 54-year-old Alaskan female with psoriatic arthritis treated with IXE for 16 weeks was seen by an outside hospital for concern of colitis. She reported a 4-week history of worsening abdominal pain, bloody diarrhea, and weight loss. Initial labs were significant for CRP 5.83 mg/dL and FC 3650 mcg/g. Five months after symptom onset, she underwent colonoscopy with General Surgery due to lack of healthcare access. Endoscopy revealed marked erythema, friability, and ulcerations, greatest in the right colon with terminal ileum sparring. She was admitted and started on extremely high dose IV methylprednisolone without symptom improvement requiring infliximab rescue therapy. Her course was immediately complicated by bowel perforation requiring right hemicolectomy and ileostomy. Histopathology revealed severe acute transmural inflammation and granulomata, consistent with Crohn’s disease. Her postoperative course was complicated by wound dehiscence and intraabdominal abscesses in the setting of significant immunosuppression and malnutrition. Ultimately, she was transferred to our institution for higher-level of care and now remains in deep remission following antibiotics and discontinuation of all immunosuppressive agents.
Discussion: This case highlights the ever-problematic healthcare disparities rural Americans face. There remains a gap in medical knowledge and experience managing this infrequent adverse association between IL-17 inhibitors and IBD. The literature lacks consensus recommendations regarding this disease entity and providers must rely on case studies for guidance. We propose a standardized approach to guide clinicians through the pretherapy, surveillance, diagnosis, and management phases of care. This work should serve to further bolster the medical literature and improve patient safety outcomes.

Disclosures:
Taylor L. Spiewak, 1, Ted A. Spiewak, DO2. P1013 - Ixekizumab-Induced Inflammatory Bowel Disease Catastrophe in the Last Frontier, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Advocate Christ Medical Center, Oak Lawn, IL; 2United States Air Force, Anchorage, AK
Introduction: Patients with psoriatic arthritis have been shown to have a 1-4-fold increased risk, compared to the general population, of developing inflammatory bowel disease (IBD). Ixekizumab (IXE) is one of four monoclonal antibodies targeting interleukin-17 or its receptor, widely used for the treatment of several immune-mediated inflammatory conditions. Despite being reported as rare (< 1%) in clinical trials, cases of new onset and exacerbation of IBD continue to be reported in real-world settings. We report a challenging case with several important learning points of de novo development of severe, complicated Crohn’s disease in a patient on IXE.
Case Description/Methods: 54-year-old Alaskan female with psoriatic arthritis treated with IXE for 16 weeks was seen by an outside hospital for concern of colitis. She reported a 4-week history of worsening abdominal pain, bloody diarrhea, and weight loss. Initial labs were significant for CRP 5.83 mg/dL and FC 3650 mcg/g. Five months after symptom onset, she underwent colonoscopy with General Surgery due to lack of healthcare access. Endoscopy revealed marked erythema, friability, and ulcerations, greatest in the right colon with terminal ileum sparring. She was admitted and started on extremely high dose IV methylprednisolone without symptom improvement requiring infliximab rescue therapy. Her course was immediately complicated by bowel perforation requiring right hemicolectomy and ileostomy. Histopathology revealed severe acute transmural inflammation and granulomata, consistent with Crohn’s disease. Her postoperative course was complicated by wound dehiscence and intraabdominal abscesses in the setting of significant immunosuppression and malnutrition. Ultimately, she was transferred to our institution for higher-level of care and now remains in deep remission following antibiotics and discontinuation of all immunosuppressive agents.
Discussion: This case highlights the ever-problematic healthcare disparities rural Americans face. There remains a gap in medical knowledge and experience managing this infrequent adverse association between IL-17 inhibitors and IBD. The literature lacks consensus recommendations regarding this disease entity and providers must rely on case studies for guidance. We propose a standardized approach to guide clinicians through the pretherapy, surveillance, diagnosis, and management phases of care. This work should serve to further bolster the medical literature and improve patient safety outcomes.

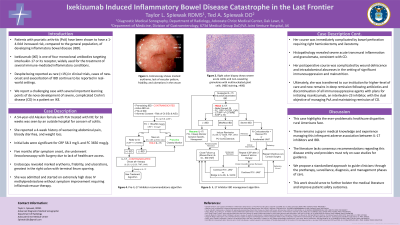
Figure: Figure 1. CT Abdomen and Pelvis. Mild circumferential colon wall thickening extending from descending colon to cecum, greatest at the splenic flexure.
Figure 2. Colonoscopy, Cecum. Inflammatory changes characterized by marked erythema, lack of vascular pattern, friability, and ulcerations.
Figure 3. Colon, Right, Segmental resection (400x). Severe acute colitis and non-caseating granuloma with multinucleated giant cells.
Figure 2. Colonoscopy, Cecum. Inflammatory changes characterized by marked erythema, lack of vascular pattern, friability, and ulcerations.
Figure 3. Colon, Right, Segmental resection (400x). Severe acute colitis and non-caseating granuloma with multinucleated giant cells.
Disclosures:
Taylor Spiewak indicated no relevant financial relationships.
Ted Spiewak indicated no relevant financial relationships.
Taylor L. Spiewak, 1, Ted A. Spiewak, DO2. P1013 - Ixekizumab-Induced Inflammatory Bowel Disease Catastrophe in the Last Frontier, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
