Sunday Poster Session
Category: IBD
P1016 - Cytomegalovirus Colitis Mimicking Steroid-Refractory Ulcerative Colitis in an Immunocompetent Elderly Patient
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Amil Shah, DO
Parkview Medical Center
Pueblo, CO
Presenting Author(s)
Amil Shah, DO1, Uday Patel, DO1, Bryant Javier, DO1, Simran Kumari, MBBS2, Kumari Priyanka, MD1, Lirio Polintan, MD1
1Parkview Medical Center, Pueblo, CO; 2Peoples University of Medical and Health Sciences for Women, Karachi, Sindh, Pakistan
Introduction: Cytomegalovirus (CMV) colitis is a significant infectious complication predominantly seen in immunocompromised patients, but can also rarely be seen in immunocompetent individuals. Clinical presentation includes diarrhea, rectal bleeding, abdominal pain and fever. Diagnosis involves endoscopic examination and biopsy, while treatment includes antiviral therapy and adjustments in immunosuppressive regimens. This case report highlights the importance of considering CMV colitis as a differential diagnosis in immunocompetent individuals whose IBD symptoms are refractory to steroids.
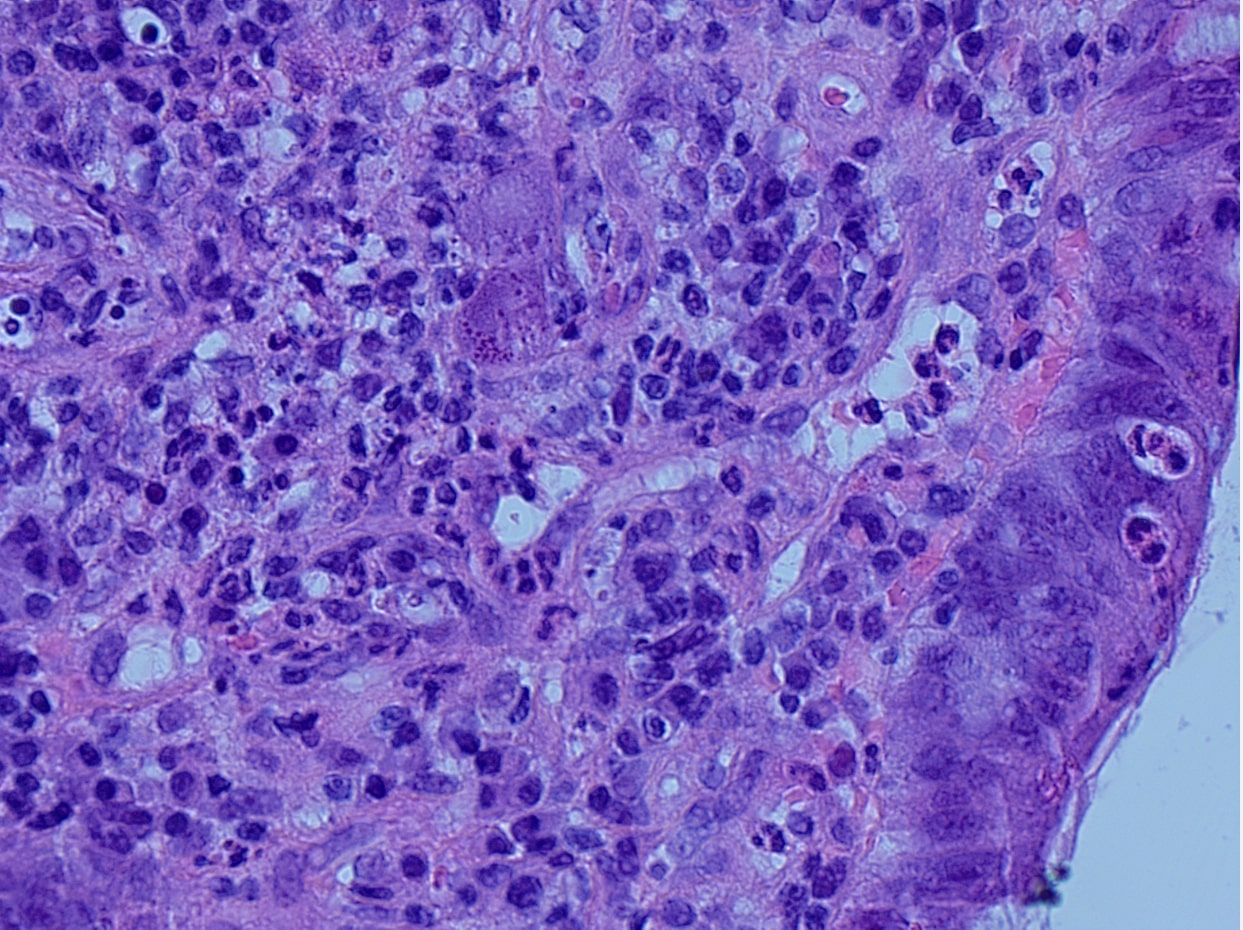
Case Description/Methods: 76-year-old female with a history of recently diagnosed ulcerative colitis who presented with right lower quadrant crampy abdominal pain, diarrhea, and hematochezia. After being diagnosed with ulcerative colitis a few weeks prior, she was discharged on a short course of prednisone. Biopsy at that time showed focal cryptitis and crypt abscesses with active and chronic proctitis. She is otherwise immunocompetent. She was readmitted due to refractory symptoms. Labs showed CRP 36, ESR 5, fecal calprotectin 990. Hepatitis panel, HIV, TB, C. difficile, GI PCR were all negative. CT abdomen was unremarkable.. She was started on methylprednisolone and infliximab, and endoscopy was scheduled. Flexible sigmoidoscopy showed mucosal ulcerations from the rectum to the descending colon with severe ulcerative colitis concerning for superinfection given worsening of inflammation despite treatment with steroids. Biopsies showed eosinophilic inclusions highly suspicious for CMV colitis. CMV PCR was positive. She was started on IV ganciclovir and transitioned to oral valganciclovir for 3 additional weeks. She was unable to start mesalamine for her ulcerative colitis due to cost. Following treatment, symptoms did not improve and repeat colonoscopy showed multiple inflammatory polyps as well as ulcerations and erosions. Biopsy showed chronic colitis, without evidence of CMV. She is currently being treated with balsalazide with plans to follow up with repeat colonoscopy in 6 months.
Discussion: Given the similar clinical and pathological characteristics of CMV colitis and IBD, and the potential concurrent presence of CMV colitis and idiopathic colitis, it is essential to consider CMV in the differential diagnosis to ensure timely and appropriate intervention. The patient’s inability to afford mesalamine also emphasizes the role of socioeconomic factors in managing her IBD, potentially impacting treatment outcomes.
Disclosures:
Amil Shah, DO1, Uday Patel, DO1, Bryant Javier, DO1, Simran Kumari, MBBS2, Kumari Priyanka, MD1, Lirio Polintan, MD1. P1016 - Cytomegalovirus Colitis Mimicking Steroid-Refractory Ulcerative Colitis in an Immunocompetent Elderly Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Parkview Medical Center, Pueblo, CO; 2Peoples University of Medical and Health Sciences for Women, Karachi, Sindh, Pakistan
Introduction: Cytomegalovirus (CMV) colitis is a significant infectious complication predominantly seen in immunocompromised patients, but can also rarely be seen in immunocompetent individuals. Clinical presentation includes diarrhea, rectal bleeding, abdominal pain and fever. Diagnosis involves endoscopic examination and biopsy, while treatment includes antiviral therapy and adjustments in immunosuppressive regimens. This case report highlights the importance of considering CMV colitis as a differential diagnosis in immunocompetent individuals whose IBD symptoms are refractory to steroids.
Case Description/Methods: 76-year-old female with a history of recently diagnosed ulcerative colitis who presented with right lower quadrant crampy abdominal pain, diarrhea, and hematochezia. After being diagnosed with ulcerative colitis a few weeks prior, she was discharged on a short course of prednisone. Biopsy at that time showed focal cryptitis and crypt abscesses with active and chronic proctitis. She is otherwise immunocompetent. She was readmitted due to refractory symptoms. Labs showed CRP 36, ESR 5, fecal calprotectin 990. Hepatitis panel, HIV, TB, C. difficile, GI PCR were all negative. CT abdomen was unremarkable.. She was started on methylprednisolone and infliximab, and endoscopy was scheduled. Flexible sigmoidoscopy showed mucosal ulcerations from the rectum to the descending colon with severe ulcerative colitis concerning for superinfection given worsening of inflammation despite treatment with steroids. Biopsies showed eosinophilic inclusions highly suspicious for CMV colitis. CMV PCR was positive. She was started on IV ganciclovir and transitioned to oral valganciclovir for 3 additional weeks. She was unable to start mesalamine for her ulcerative colitis due to cost. Following treatment, symptoms did not improve and repeat colonoscopy showed multiple inflammatory polyps as well as ulcerations and erosions. Biopsy showed chronic colitis, without evidence of CMV. She is currently being treated with balsalazide with plans to follow up with repeat colonoscopy in 6 months.
Discussion: Given the similar clinical and pathological characteristics of CMV colitis and IBD, and the potential concurrent presence of CMV colitis and idiopathic colitis, it is essential to consider CMV in the differential diagnosis to ensure timely and appropriate intervention. The patient’s inability to afford mesalamine also emphasizes the role of socioeconomic factors in managing her IBD, potentially impacting treatment outcomes.
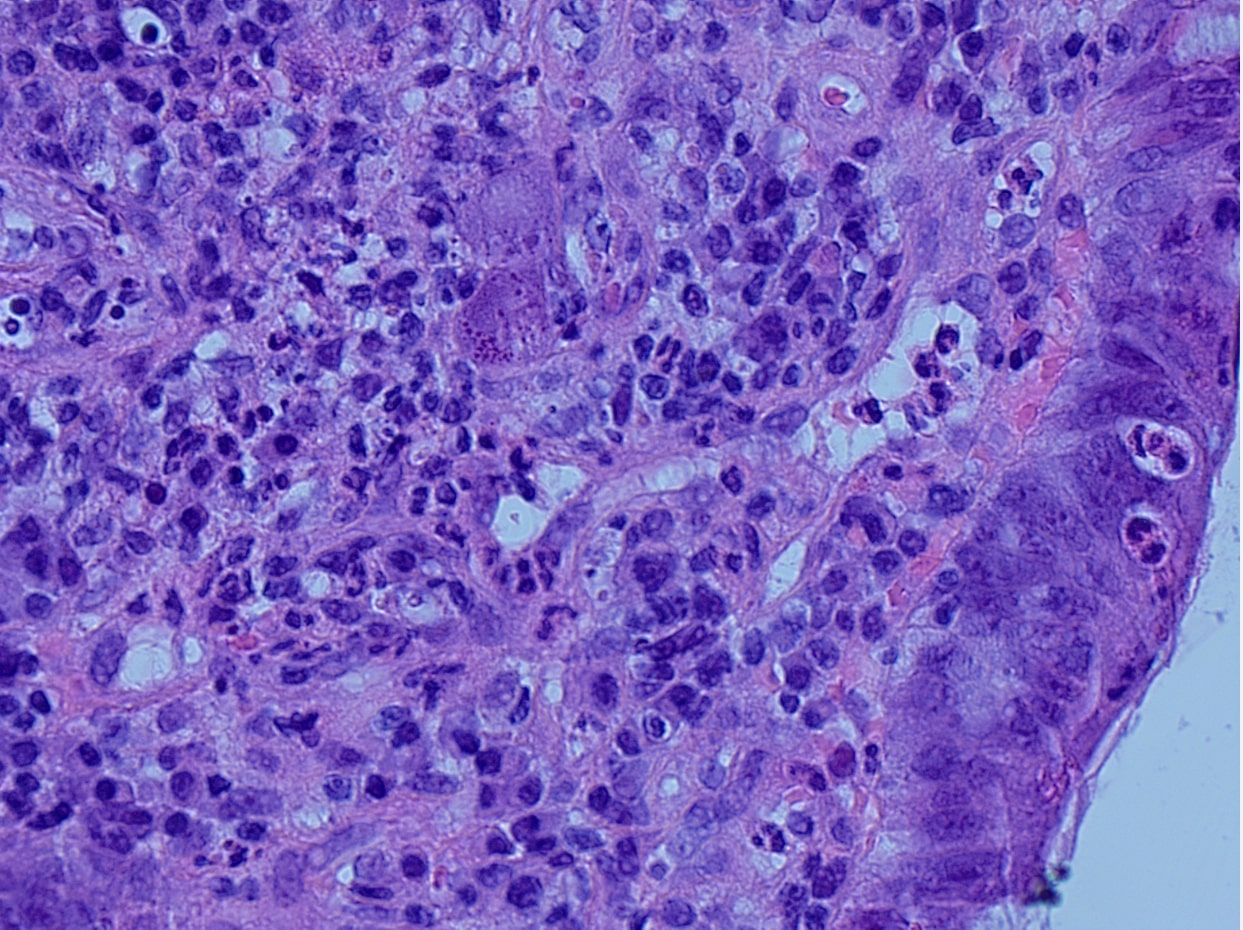
Figure: Eosinophilic inclusions, large atypical cells with intranuclear inclusion bodies or "owl-eye appearance"
Disclosures:
Amil Shah indicated no relevant financial relationships.
Uday Patel indicated no relevant financial relationships.
Bryant Javier indicated no relevant financial relationships.
Simran Kumari indicated no relevant financial relationships.
Kumari Priyanka indicated no relevant financial relationships.
Lirio Polintan indicated no relevant financial relationships.
Amil Shah, DO1, Uday Patel, DO1, Bryant Javier, DO1, Simran Kumari, MBBS2, Kumari Priyanka, MD1, Lirio Polintan, MD1. P1016 - Cytomegalovirus Colitis Mimicking Steroid-Refractory Ulcerative Colitis in an Immunocompetent Elderly Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
