Sunday Poster Session
Category: IBD
P1017 - Hiding In Plain Sight: A Case of Concurrent Pustular Psoriasis and Inflammatory Bowel Disease
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- RS
Robinderpal Sandhu, DO
Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Robinderpal Sandhu, DO1, Emily Seltzer, DO, MS2, Binoy Desai, DO2, Mantej Sehmbhi, MBBS2, Michael S.. Smith, MD, MBA3
1Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 3Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Psoriasis and Inflammatory Bowel Disease (IBD) are both chronic, relapsing and remitting inflammatory conditions. Individuals with both pustular psoriasis and IBD comprise a unique patient population. Symptom presentation can include fevers, arthralgias, characteristic skin lesions and abdominal pain.
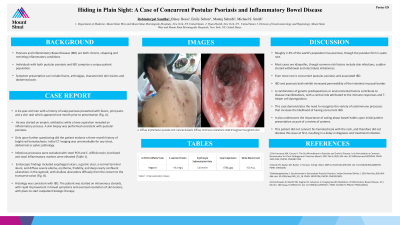
Case Description/Methods: A 24-year-old man with a history of scalp psoriasis presented with fevers, joint pains and a skin rash which appeared one month prior to presentation (Fig. A). He was started on empiric antibiotics while a knee aspiration revealed an inflammatory process. A skin biopsy was performed consistent with pustular psoriasis.
Only upon further questioning did the patient endorse a three month history of bright red hematochezia. Initial CT imaging was unremarkable for any chest, abdominal or pelvic pathology. Infectious processes were excluded with stool PCR and C. difficile toxin, but blood and stool inflammatory markers were elevated (Table 1). Endoscopic findings included esophageal ulcers, a gastric ulcer, a normal terminal ileum, and diffuse severe edema, erythema, friability, and deep nearly confluent ulcerations in the sigmoid, with shallow ulcerations diffusely from the rectum to the transverse colon (Fig. B). Histology was consistent with IBD. The patient was started on intravenous steroids, with rapid improvement in bowel symptoms and eventual resolution of skin lesions, with plans to start outpatient biologic therapy.
Discussion: Roughly 2-3% of the world’s population has psoriasis, though the pustular form is quite rare. Most cases are idiopathic, though common risk factors include skin infections, sudden steroid withdrawal and electrolyte imbalances. Even more rare is concurrent pustular psoriasis and associated IBD.
IBD and psoriasis both exhibit increased permeability of the intestinal mucosal border. A combination of genetic predispositions or environmental factors contribute to disease manifestations, with a central role attributed to the immune responses and T-helper cell dysregulation. This case demonstrates the need to recognize the variety of autoimmune processes that increase the likelihood of having concurrent IBD. It also underscores the importance of asking about bowel habits upon initial patient presentation as part of a review of systems. This patient did not connect his hematochezia with the rash, and therefore did not disclose this issue at first, resulting in a delay in diagnosis and treatment initiation.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Robinderpal Sandhu, DO1, Emily Seltzer, DO, MS2, Binoy Desai, DO2, Mantej Sehmbhi, MBBS2, Michael S.. Smith, MD, MBA3. P1017 - Hiding In Plain Sight: A Case of Concurrent Pustular Psoriasis and Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY; 3Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Psoriasis and Inflammatory Bowel Disease (IBD) are both chronic, relapsing and remitting inflammatory conditions. Individuals with both pustular psoriasis and IBD comprise a unique patient population. Symptom presentation can include fevers, arthralgias, characteristic skin lesions and abdominal pain.
Case Description/Methods: A 24-year-old man with a history of scalp psoriasis presented with fevers, joint pains and a skin rash which appeared one month prior to presentation (Fig. A). He was started on empiric antibiotics while a knee aspiration revealed an inflammatory process. A skin biopsy was performed consistent with pustular psoriasis.
Only upon further questioning did the patient endorse a three month history of bright red hematochezia. Initial CT imaging was unremarkable for any chest, abdominal or pelvic pathology. Infectious processes were excluded with stool PCR and C. difficile toxin, but blood and stool inflammatory markers were elevated (Table 1). Endoscopic findings included esophageal ulcers, a gastric ulcer, a normal terminal ileum, and diffuse severe edema, erythema, friability, and deep nearly confluent ulcerations in the sigmoid, with shallow ulcerations diffusely from the rectum to the transverse colon (Fig. B). Histology was consistent with IBD. The patient was started on intravenous steroids, with rapid improvement in bowel symptoms and eventual resolution of skin lesions, with plans to start outpatient biologic therapy.
Discussion: Roughly 2-3% of the world’s population has psoriasis, though the pustular form is quite rare. Most cases are idiopathic, though common risk factors include skin infections, sudden steroid withdrawal and electrolyte imbalances. Even more rare is concurrent pustular psoriasis and associated IBD.
IBD and psoriasis both exhibit increased permeability of the intestinal mucosal border. A combination of genetic predispositions or environmental factors contribute to disease manifestations, with a central role attributed to the immune responses and T-helper cell dysregulation. This case demonstrates the need to recognize the variety of autoimmune processes that increase the likelihood of having concurrent IBD. It also underscores the importance of asking about bowel habits upon initial patient presentation as part of a review of systems. This patient did not connect his hematochezia with the rash, and therefore did not disclose this issue at first, resulting in a delay in diagnosis and treatment initiation.

Figure: A. Diffuse, erythematous pustules with ruptured bullae B. Diffuse, continuous ulcerations noted throughout the sigmoid colon
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Robinderpal Sandhu indicated no relevant financial relationships.
Emily Seltzer indicated no relevant financial relationships.
Binoy Desai indicated no relevant financial relationships.
Mantej Sehmbhi indicated no relevant financial relationships.
Michael Smith: Castle Biosciences – Advisory Committee/Board Member, Consultant. CDx Diagnostics – Consultant. Lucid Diagnostics – Advisory Committee/Board Member, Consultant. Provation Medical – Consultant. Steris Endoscopy – Advisory Committee/Board Member, Consultant.
Robinderpal Sandhu, DO1, Emily Seltzer, DO, MS2, Binoy Desai, DO2, Mantej Sehmbhi, MBBS2, Michael S.. Smith, MD, MBA3. P1017 - Hiding In Plain Sight: A Case of Concurrent Pustular Psoriasis and Inflammatory Bowel Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

