Sunday Poster Session
Category: IBD
P1018 - A Clinical Conundrum: Journey to a Diagnosis of Esophageal Crohn’s
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- SB
Sonya Bhaskar, MD
University of South Florida
Tampa, FL
Presenting Author(s)
Sonya Bhaskar, MD1, John Jacobs, MD, FACG2, Michelle Rosario, MD2
1University of South Florida, Tampa, FL; 2University of South Florida Morsani College of Medicine, Tampa, FL
Introduction: Esophageal involvement in Crohn’s disease is rare. Diagnosis can be difficult given the rarity of the disease and nonspecific findings. Here we present an unusual case of a patient with long-standing dysphagia with high suspicion for esophageal Crohn’s disease.
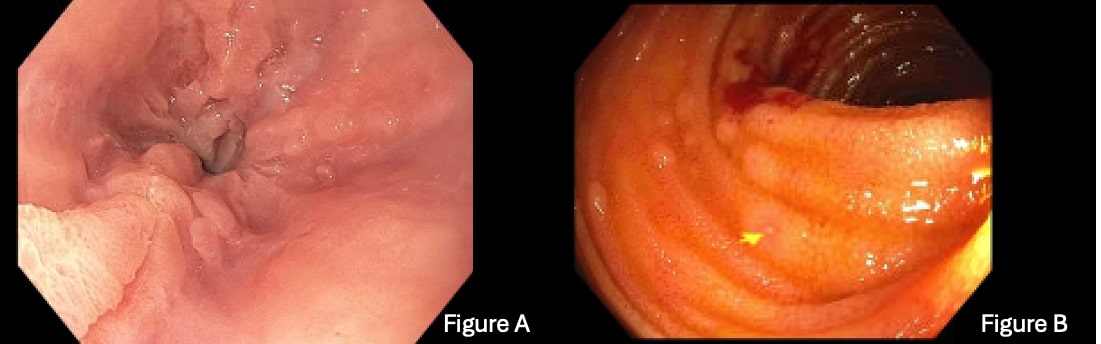
Case Description/Methods: A 25-year-old male presented with progressive solid food dysphagia for six years. His initial esophagogastroduodenoscopy (EGD) revealed abnormal mucosa in the distal esophagus associated with an esophageal stenosis. The mucosa was circumferential, friable, frond-like, and spongy appearing with heaped up edges and punched-out lesions (Figure A). The patient underwent dilation and biopsies in Michel’s fixative noted a prominent lymphocytic infiltrate involving the epithelium and interface of lamina propria and scattered dyskeratotic keratinocytes which was felt to be more consistent with lichen planus. He was treated with aceterin with no improvement. The patient had multiple dilations every 1-2 months. In subsequent EGDs, an increase in eosinophils in gastric and duodenal biopsies was noted and he was diagnosed with eosinophilic gastritis and enteritis. His eosinophil count improved with proton pump therapy and an elimination diet. He had endoscopic improvement with a course of prednisone; however he still was requiring frequent dilation. On his last EGD, pathology noted a few poorly formed granulomas in the stomach. Since his colonoscopy showed one aphthous ulcer in his terminal ileum (Figure B), the diagnosis was changed to Crohn’s disease. The patient was started on Infliximab (IFX), Methotrexate (MTX) and Budesonide slurry.
Discussion: The main presenting symptoms for esophageal Crohn’s are dysphagia, odynophagia and epigastric pain. Endoscopic findings are variable and include friability, aphthoid and “punched-out” ulcers, cobblestone appearance, masses, stenoses, and fistulas often in the middle and distal third of the esophagus. Diagnosis is difficult as the common histological findings are nonspecific chronic inflammation, and a lymphocytic infiltrate in the lamina propria. Superficial biopsies might not be sufficient to identify granulomas and are observed in less than 25% of cases. Treatment of esophageal Crohn’s can involve acid suppressive therapy and corticosteroids in milder disease and immunomodulatory therapy in severe disease. Given our patient’s severe presentation and recurrent need for dilation, the decision was made to pursue dual immunosuppression.
Disclosures:
Sonya Bhaskar, MD1, John Jacobs, MD, FACG2, Michelle Rosario, MD2. P1018 - A Clinical Conundrum: Journey to a Diagnosis of Esophageal Crohn’s, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of South Florida, Tampa, FL; 2University of South Florida Morsani College of Medicine, Tampa, FL
Introduction: Esophageal involvement in Crohn’s disease is rare. Diagnosis can be difficult given the rarity of the disease and nonspecific findings. Here we present an unusual case of a patient with long-standing dysphagia with high suspicion for esophageal Crohn’s disease.
Case Description/Methods: A 25-year-old male presented with progressive solid food dysphagia for six years. His initial esophagogastroduodenoscopy (EGD) revealed abnormal mucosa in the distal esophagus associated with an esophageal stenosis. The mucosa was circumferential, friable, frond-like, and spongy appearing with heaped up edges and punched-out lesions (Figure A). The patient underwent dilation and biopsies in Michel’s fixative noted a prominent lymphocytic infiltrate involving the epithelium and interface of lamina propria and scattered dyskeratotic keratinocytes which was felt to be more consistent with lichen planus. He was treated with aceterin with no improvement. The patient had multiple dilations every 1-2 months. In subsequent EGDs, an increase in eosinophils in gastric and duodenal biopsies was noted and he was diagnosed with eosinophilic gastritis and enteritis. His eosinophil count improved with proton pump therapy and an elimination diet. He had endoscopic improvement with a course of prednisone; however he still was requiring frequent dilation. On his last EGD, pathology noted a few poorly formed granulomas in the stomach. Since his colonoscopy showed one aphthous ulcer in his terminal ileum (Figure B), the diagnosis was changed to Crohn’s disease. The patient was started on Infliximab (IFX), Methotrexate (MTX) and Budesonide slurry.
Discussion: The main presenting symptoms for esophageal Crohn’s are dysphagia, odynophagia and epigastric pain. Endoscopic findings are variable and include friability, aphthoid and “punched-out” ulcers, cobblestone appearance, masses, stenoses, and fistulas often in the middle and distal third of the esophagus. Diagnosis is difficult as the common histological findings are nonspecific chronic inflammation, and a lymphocytic infiltrate in the lamina propria. Superficial biopsies might not be sufficient to identify granulomas and are observed in less than 25% of cases. Treatment of esophageal Crohn’s can involve acid suppressive therapy and corticosteroids in milder disease and immunomodulatory therapy in severe disease. Given our patient’s severe presentation and recurrent need for dilation, the decision was made to pursue dual immunosuppression.
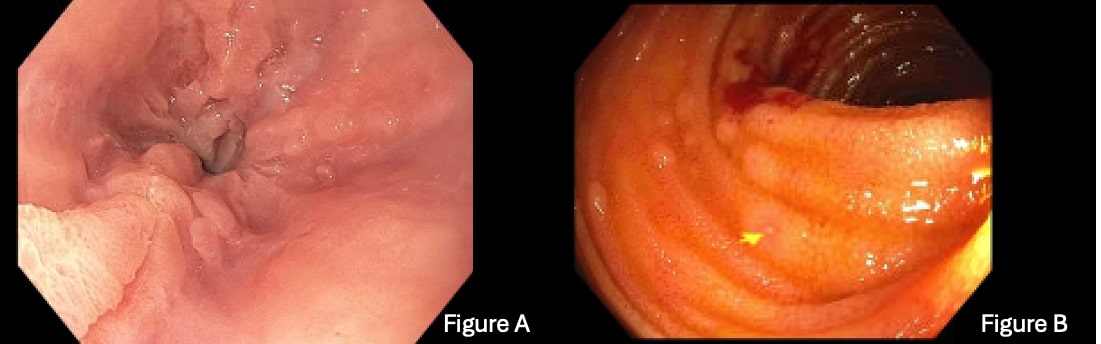
Figure: Figure A: Distal esophageal stenosis with friable, frond-like, and spongy appearance with heaped up edges and punched-out lesions
Figure B: Aphthous Ulcer in the terminal ileum. Biopsies were normal
Figure B: Aphthous Ulcer in the terminal ileum. Biopsies were normal
Disclosures:
Sonya Bhaskar indicated no relevant financial relationships.
John Jacobs: Medtronic – Consultant. Regeneron – Speakers Bureau. Sanofi/Genzyme – Speakers Bureau.
Michelle Rosario: Abbvie – Speakers Bureau.
Sonya Bhaskar, MD1, John Jacobs, MD, FACG2, Michelle Rosario, MD2. P1018 - A Clinical Conundrum: Journey to a Diagnosis of Esophageal Crohn’s, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
