Sunday Poster Session
Category: IBD
P1019 - From Gut Flare to Cardiac Scare: A Case of Crohn's Myopericarditis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- CN
Chydubem Nwaiwu, MD
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
Chydubem Nwaiwu, MD1, Alexandra Fiedler, MD1, Giovanni Vertus, 2, Sarah Malik, MD1
1University of Nebraska Medical Center, Omaha, NE; 2Ross University School of Medicine, Miami Lkaes, FL
Introduction: Crohn's disease (CD) is a chronic inflammatory bowel condition with various extraintestinal manifestations, including the rare but serious complication of Crohn’s Myopericarditis (CM). CM requires prompt diagnosis and management due to its potential severity. This case involves a middle-aged female with CM complicated by shock, highlighting the need for high vigilance in critically ill CD patients.
Case Description/Methods: A 44-year-old female with an 8-year history of CD presented with substernal pleuritic chest pain, worsened by lying down. She was hypotensive at 92/51 mmHg and reported 10 bloody bowel movements prior. Previously on Mesalamine and Budesonide, she had discontinued these medications two years prior. Her EKG showed T-wave changes in the anterior leads. Laboratory tests revealed elevated troponins (peaking at 89 ng/dL, normal < 16 ng/dL), Chronic Heart Failure peptide (1030 pg/ml, normal 0-100 pg/ml), Erythrocyte Sedimentation Rate (31 mm/hr, normal 0-20 mm/hr), and C-Reactive Protein (16.5 mg/dL, normal < 1 mg/dL). Fecal calprotectin was >8000 micrograms/mL (normal < 50 micrograms/mL), and the gastrointestinal pathogen panel was negative.
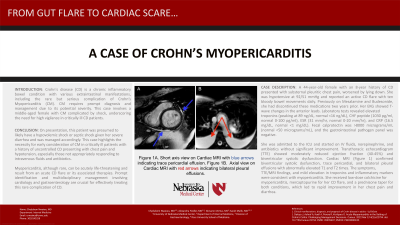
She was admitted to the intensive care unit and started on intravenous (IV) fluids, norepinephrine, and antibiotics without significant improvement. Transthoracic echocardiogram (TTE) showed moderately reduced ejection fraction (40-45%) and biventricular systolic dysfunction. Cardiac Magnetic Resonance Imaging (MRI) showed trace pericardial, and bilateral pleural effusions (Figure 1) with elevated T1 and T2 times. Her symptoms, TTE/MRI findings, mild elevation in troponins and inflammatory markers were consistent with myopericarditis. She received low-dose colchicine for myopericarditis, mercaptopurine for her CD flare, and a prednisone taper for both conditions, which rapidly improved her chest pain and diarrhea.
Discussion: This patient, presumed to likely have hypovolemic or septic shock, was managed accordingly. This case underscores the necessity for early consideration of CM in critically ill patients with a history of uncontrolled CD presenting with chest pain and hypotension, especially those not appropriately responding to IV fluids and antibiotics. Myopericarditis, although rare, can be acutely life-threatening and result from an acute CD flare or its associated therapies. Prompt identification and multidisciplinary management involving cardiology and gastroenterology are crucial for effectively treating this rare complication of CD.

Disclosures:
Chydubem Nwaiwu, MD1, Alexandra Fiedler, MD1, Giovanni Vertus, 2, Sarah Malik, MD1. P1019 - From Gut Flare to Cardiac Scare: A Case of Crohn's Myopericarditis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Nebraska Medical Center, Omaha, NE; 2Ross University School of Medicine, Miami Lkaes, FL
Introduction: Crohn's disease (CD) is a chronic inflammatory bowel condition with various extraintestinal manifestations, including the rare but serious complication of Crohn’s Myopericarditis (CM). CM requires prompt diagnosis and management due to its potential severity. This case involves a middle-aged female with CM complicated by shock, highlighting the need for high vigilance in critically ill CD patients.
Case Description/Methods: A 44-year-old female with an 8-year history of CD presented with substernal pleuritic chest pain, worsened by lying down. She was hypotensive at 92/51 mmHg and reported 10 bloody bowel movements prior. Previously on Mesalamine and Budesonide, she had discontinued these medications two years prior. Her EKG showed T-wave changes in the anterior leads. Laboratory tests revealed elevated troponins (peaking at 89 ng/dL, normal < 16 ng/dL), Chronic Heart Failure peptide (1030 pg/ml, normal 0-100 pg/ml), Erythrocyte Sedimentation Rate (31 mm/hr, normal 0-20 mm/hr), and C-Reactive Protein (16.5 mg/dL, normal < 1 mg/dL). Fecal calprotectin was >8000 micrograms/mL (normal < 50 micrograms/mL), and the gastrointestinal pathogen panel was negative.
She was admitted to the intensive care unit and started on intravenous (IV) fluids, norepinephrine, and antibiotics without significant improvement. Transthoracic echocardiogram (TTE) showed moderately reduced ejection fraction (40-45%) and biventricular systolic dysfunction. Cardiac Magnetic Resonance Imaging (MRI) showed trace pericardial, and bilateral pleural effusions (Figure 1) with elevated T1 and T2 times. Her symptoms, TTE/MRI findings, mild elevation in troponins and inflammatory markers were consistent with myopericarditis. She received low-dose colchicine for myopericarditis, mercaptopurine for her CD flare, and a prednisone taper for both conditions, which rapidly improved her chest pain and diarrhea.
Discussion: This patient, presumed to likely have hypovolemic or septic shock, was managed accordingly. This case underscores the necessity for early consideration of CM in critically ill patients with a history of uncontrolled CD presenting with chest pain and hypotension, especially those not appropriately responding to IV fluids and antibiotics. Myopericarditis, although rare, can be acutely life-threatening and result from an acute CD flare or its associated therapies. Prompt identification and multidisciplinary management involving cardiology and gastroenterology are crucial for effectively treating this rare complication of CD.

Figure: Figure 1A. Short axis view on Cardiac MRI with blue arrows indicating trace pericardial effusion. Figure 1B. Axial view on Cardiac MRI with red arrows indicating bilateral pleural effusions.
Disclosures:
Chydubem Nwaiwu indicated no relevant financial relationships.
Alexandra Fiedler indicated no relevant financial relationships.
Giovanni Vertus indicated no relevant financial relationships.
Sarah Malik indicated no relevant financial relationships.
Chydubem Nwaiwu, MD1, Alexandra Fiedler, MD1, Giovanni Vertus, 2, Sarah Malik, MD1. P1019 - From Gut Flare to Cardiac Scare: A Case of Crohn's Myopericarditis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
