Sunday Poster Session
Category: Interventional Endoscopy
P1118 - Challenges in Managing Hemobilia Post-ERCP: A Case of Ulceration and Successful Intervention
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Aastha Bharwad, MD
University of Texas at Houston
Houston, TX
Presenting Author(s)
Aastha Bharwad, MD1, Hasan Jaber, MD2, Lawrence Zhou, MD3, Stephanie J. Melquist, MD4, William J. Salyers, MD, MPH4
1University of Texas at Houston, Houston, TX; 2University of Kansas Medical Center, Wichita, KS; 3The University of Kansas School of Medicine, Wichita, KS; 4University of Kansas School of Medicine, Wichita, KS
Introduction: Biliary endoscopic sphincterotomy (EST) plays a crucial role in managing a broad range of biliary and papillary disorders through endoscopic retrograde cholangiopancreatography (ERCP). Despite its importance in treating obstructive pathologies, EST carries risks, including hemobilia—a rare but significant cause of gastrointestinal (GI) bleeding. Hemobilia often stems from iatrogenic factors associated with invasive interventions within the hepatopancreatobiliary system.
Our case highlights the challenge of managing patients with nonspecific symptoms following recent hepatopancreatobiliary interventions, exemplified by an ulceration at a prior sphincterotomy site with a visible vessel.
Case Description/Methods: A 29-year-old woman with a recent history of choledocholithiasis and cholecystitis, treated with laparoscopic cholecystectomy and ERCP with complete removal of stone with biliary sphincterotomy and balloon extraction, returned two days later with symptoms of abdominal discomfort, nausea, vomiting, and dark stools.
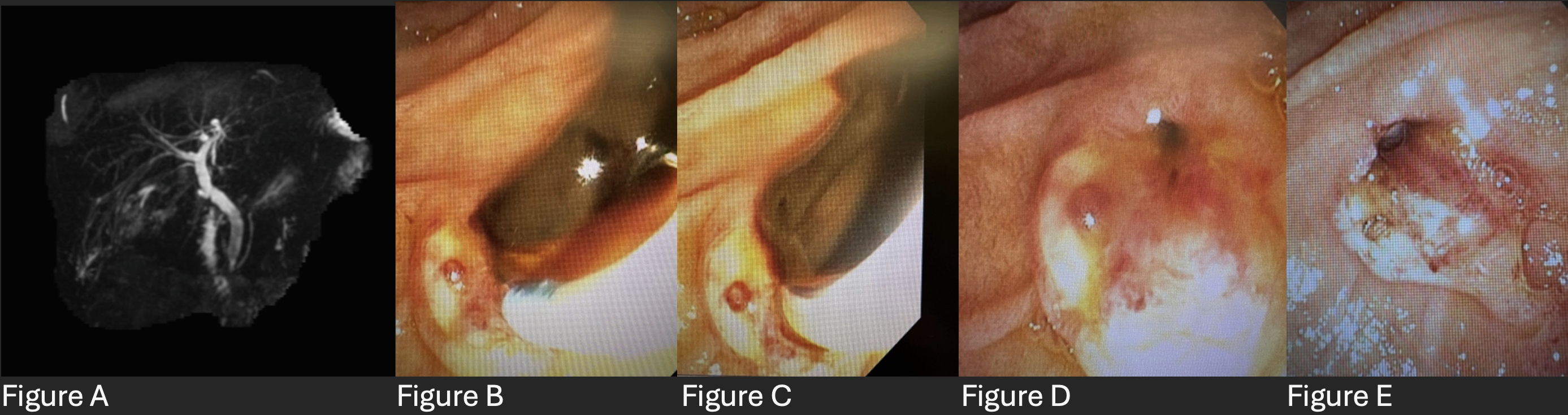
Labs showed leukocytosis, elevated transaminases, bilirubin, and alkaline phosphatase. Her hemoglobin declined from 14.5 to 9.1 gm/dL during hospitalization without requiring transfusion. Computed Tomography (CT) revealed pneumoperitoneum consistent with recent surgery. Magnetic resonance cholangiopancreatography (MRCP) showed common bile duct (CBD) filling defects with minimal dilation of 8-9mm in diameter (Figure A).
ERCP was repeated for suspicion of hemobilia, and the major papilla was found to be ulcerated at the prior sphincterotomy site with a visible vessel present in the base of ulcer. A sphincterotome was passed over the guidewire and bile duct was deeply cannulated. The main bile duct was moderately dilated, and the lower third contained filling defects. Bile duct dilation with balloon dilator and clot removal were successful; ensuring smooth contrast flow into the duodenum without bile leakage. Effective coagulation using a bipolar probe through ERCP scope resolved the ulcer's vessel (Figure B-E), ultimately leading to patients’ symptom resolution.
Discussion: Timely recognition of hemobilia is crucial due to its potential for severe consequences, and presentation with nonspecific symptoms including abdominal pain, upper GI bleeding, and jaundice. Effective management involves hemostasis, preservation of biliary flow, and treatment of the underlying cause while navigating complexities such as the risk of recurrent biliary obstruction and pancreatic duct injury.
Disclosures:
Aastha Bharwad, MD1, Hasan Jaber, MD2, Lawrence Zhou, MD3, Stephanie J. Melquist, MD4, William J. Salyers, MD, MPH4. P1118 - Challenges in Managing Hemobilia Post-ERCP: A Case of Ulceration and Successful Intervention, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas at Houston, Houston, TX; 2University of Kansas Medical Center, Wichita, KS; 3The University of Kansas School of Medicine, Wichita, KS; 4University of Kansas School of Medicine, Wichita, KS
Introduction: Biliary endoscopic sphincterotomy (EST) plays a crucial role in managing a broad range of biliary and papillary disorders through endoscopic retrograde cholangiopancreatography (ERCP). Despite its importance in treating obstructive pathologies, EST carries risks, including hemobilia—a rare but significant cause of gastrointestinal (GI) bleeding. Hemobilia often stems from iatrogenic factors associated with invasive interventions within the hepatopancreatobiliary system.
Our case highlights the challenge of managing patients with nonspecific symptoms following recent hepatopancreatobiliary interventions, exemplified by an ulceration at a prior sphincterotomy site with a visible vessel.
Case Description/Methods: A 29-year-old woman with a recent history of choledocholithiasis and cholecystitis, treated with laparoscopic cholecystectomy and ERCP with complete removal of stone with biliary sphincterotomy and balloon extraction, returned two days later with symptoms of abdominal discomfort, nausea, vomiting, and dark stools.
Labs showed leukocytosis, elevated transaminases, bilirubin, and alkaline phosphatase. Her hemoglobin declined from 14.5 to 9.1 gm/dL during hospitalization without requiring transfusion. Computed Tomography (CT) revealed pneumoperitoneum consistent with recent surgery. Magnetic resonance cholangiopancreatography (MRCP) showed common bile duct (CBD) filling defects with minimal dilation of 8-9mm in diameter (Figure A).
ERCP was repeated for suspicion of hemobilia, and the major papilla was found to be ulcerated at the prior sphincterotomy site with a visible vessel present in the base of ulcer. A sphincterotome was passed over the guidewire and bile duct was deeply cannulated. The main bile duct was moderately dilated, and the lower third contained filling defects. Bile duct dilation with balloon dilator and clot removal were successful; ensuring smooth contrast flow into the duodenum without bile leakage. Effective coagulation using a bipolar probe through ERCP scope resolved the ulcer's vessel (Figure B-E), ultimately leading to patients’ symptom resolution.
Discussion: Timely recognition of hemobilia is crucial due to its potential for severe consequences, and presentation with nonspecific symptoms including abdominal pain, upper GI bleeding, and jaundice. Effective management involves hemostasis, preservation of biliary flow, and treatment of the underlying cause while navigating complexities such as the risk of recurrent biliary obstruction and pancreatic duct injury.
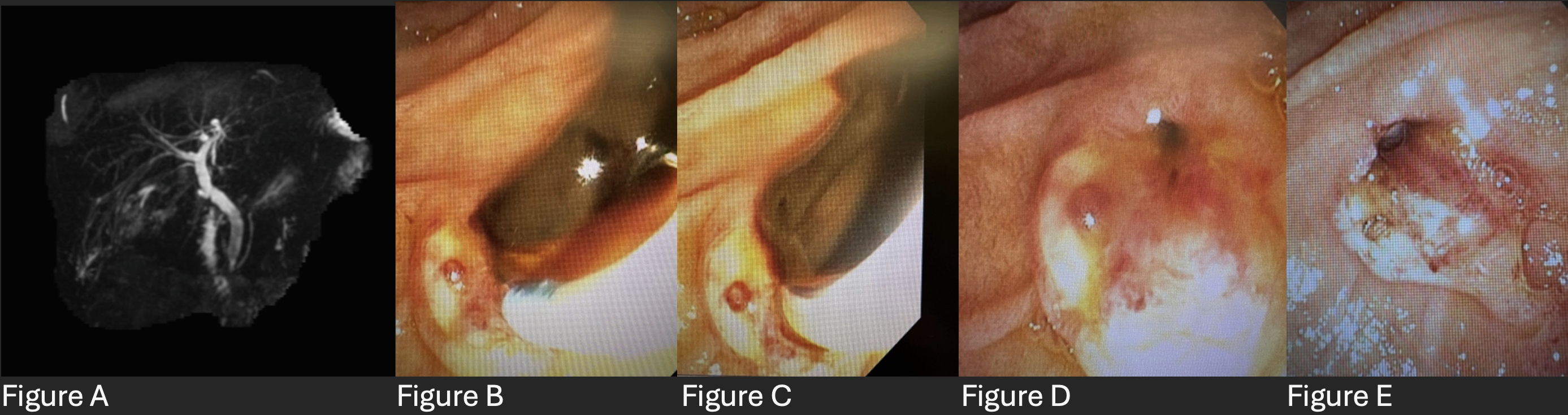
Figure: Figure A: MRCP showing common bile duct (CBD) filling defects with minimal dilation of 8-9 mm in diameter
Figure B: Sphincter with clot, pre-cannulation
Figure C: Sphincter with clot, post cannulation
Figure D: Removal of clot with small visible vessel on left
Figure E: Post-treatment with bipolar probe
Figure B: Sphincter with clot, pre-cannulation
Figure C: Sphincter with clot, post cannulation
Figure D: Removal of clot with small visible vessel on left
Figure E: Post-treatment with bipolar probe
Disclosures:
Aastha Bharwad indicated no relevant financial relationships.
Hasan Jaber indicated no relevant financial relationships.
Lawrence Zhou indicated no relevant financial relationships.
Stephanie Melquist indicated no relevant financial relationships.
William Salyers indicated no relevant financial relationships.
Aastha Bharwad, MD1, Hasan Jaber, MD2, Lawrence Zhou, MD3, Stephanie J. Melquist, MD4, William J. Salyers, MD, MPH4. P1118 - Challenges in Managing Hemobilia Post-ERCP: A Case of Ulceration and Successful Intervention, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
