Sunday Poster Session
Category: Interventional Endoscopy
P1122 - Endoscopic Ultrasound-Guided Esophagojejunal Anastomosis: A Case Series on the Novel Technique and Our Experience
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Abby Kunitsky, DO
McLaren Macomb Hospital
Mt. Clemens, MI
Presenting Author(s)
Award: Presidential Poster Award
Abby Kunitsky, DO1, Steve Siegal, MD2, Mark Bloomston, MD3, Bassan Allan, MD3, Augustine Salami, MD4
1McLaren Macomb Hospital, Mt. Clemens, MI; 2GI Surgical Specialists, Fort Myers, FL; 3South Florida Surgical Oncology, Fort Myers, FL; 4LPG Gastroenterology, Fort Myers, FL
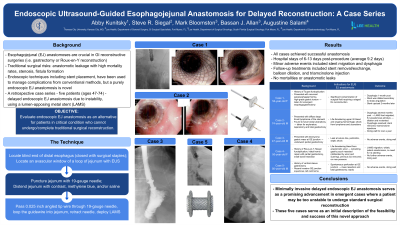
Introduction: Esophagojejunal (EJ) anastomoses are integral to gastrointestinal reconstructive surgeries following procedures like gastrectomy, particularly in cases of cancer or Roux-en-Y reconstruction. Despite their prevalence, the traditional surgical approaches can lead to adverse events such as anastomotic leakage or stenosis. While endoscopic therapies have been used for managing these complications, a primarily endoscopic EJ anastomosis technique has not yet been described. This study presents a retrospective case series detailing the use of a primarily endoscopic EJ anastomosis with lumen-apposing metal stent (LAMS) placement in five patients.
Case Description/Methods: Five patients, aged 47-74, underwent endoscopic EJ anastomosis following complications necessitating this emergent alternative approach. Each case involved significant patient instability or critical condition, such as septic/hemorrhagic shock or contamination from a life-threatening bleed, stricture, gastric torsion, or perforation. The procedures were performed by the same advanced endoscopist using endoscopic ultrasound (EUS) guidance and LAMS placement between the esophagus and jejunum. Echosonography was used against the blind loop of esophagus left in discontinuity, identifying and puncturing an avascular window of the adjacent loop of jejunum, and distending this loop of bowel with a contrast saline solution. A guidewire was then looped into the jejunum and a LAMS was deployed. Patient outcomes and follow-up were documented. The average hospital stay post-procedure ranged from 6-13 days.
Discussion: Endoscopic EJ anastomosis with LAMS placement offers an advanced minimally invasive alternative approach in managing high-risk, complex patients unable to follow through with traditional surgical reconstruction. The technique demonstrated feasibility and efficacy, with successful anastomosis achieved in all cases and, most importantly, no anastomotic leaks or mortalities. To our knowledge, this is the first human case series description of an EUS-guided endoscopic EJ anastomosis technique with placement of a stent between the esophagus and the jejunum. Further research is warranted to assess long-term efficacy and effects across a larger patient cohort. These findings contribute to the potential of advanced endoscopic techniques in improving patient outcomes and warrants further exploration and refinement.
Disclosures:
Abby Kunitsky, DO1, Steve Siegal, MD2, Mark Bloomston, MD3, Bassan Allan, MD3, Augustine Salami, MD4. P1122 - Endoscopic Ultrasound-Guided Esophagojejunal Anastomosis: A Case Series on the Novel Technique and Our Experience, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Abby Kunitsky, DO1, Steve Siegal, MD2, Mark Bloomston, MD3, Bassan Allan, MD3, Augustine Salami, MD4
1McLaren Macomb Hospital, Mt. Clemens, MI; 2GI Surgical Specialists, Fort Myers, FL; 3South Florida Surgical Oncology, Fort Myers, FL; 4LPG Gastroenterology, Fort Myers, FL
Introduction: Esophagojejunal (EJ) anastomoses are integral to gastrointestinal reconstructive surgeries following procedures like gastrectomy, particularly in cases of cancer or Roux-en-Y reconstruction. Despite their prevalence, the traditional surgical approaches can lead to adverse events such as anastomotic leakage or stenosis. While endoscopic therapies have been used for managing these complications, a primarily endoscopic EJ anastomosis technique has not yet been described. This study presents a retrospective case series detailing the use of a primarily endoscopic EJ anastomosis with lumen-apposing metal stent (LAMS) placement in five patients.
Case Description/Methods: Five patients, aged 47-74, underwent endoscopic EJ anastomosis following complications necessitating this emergent alternative approach. Each case involved significant patient instability or critical condition, such as septic/hemorrhagic shock or contamination from a life-threatening bleed, stricture, gastric torsion, or perforation. The procedures were performed by the same advanced endoscopist using endoscopic ultrasound (EUS) guidance and LAMS placement between the esophagus and jejunum. Echosonography was used against the blind loop of esophagus left in discontinuity, identifying and puncturing an avascular window of the adjacent loop of jejunum, and distending this loop of bowel with a contrast saline solution. A guidewire was then looped into the jejunum and a LAMS was deployed. Patient outcomes and follow-up were documented. The average hospital stay post-procedure ranged from 6-13 days.
Discussion: Endoscopic EJ anastomosis with LAMS placement offers an advanced minimally invasive alternative approach in managing high-risk, complex patients unable to follow through with traditional surgical reconstruction. The technique demonstrated feasibility and efficacy, with successful anastomosis achieved in all cases and, most importantly, no anastomotic leaks or mortalities. To our knowledge, this is the first human case series description of an EUS-guided endoscopic EJ anastomosis technique with placement of a stent between the esophagus and the jejunum. Further research is warranted to assess long-term efficacy and effects across a larger patient cohort. These findings contribute to the potential of advanced endoscopic techniques in improving patient outcomes and warrants further exploration and refinement.
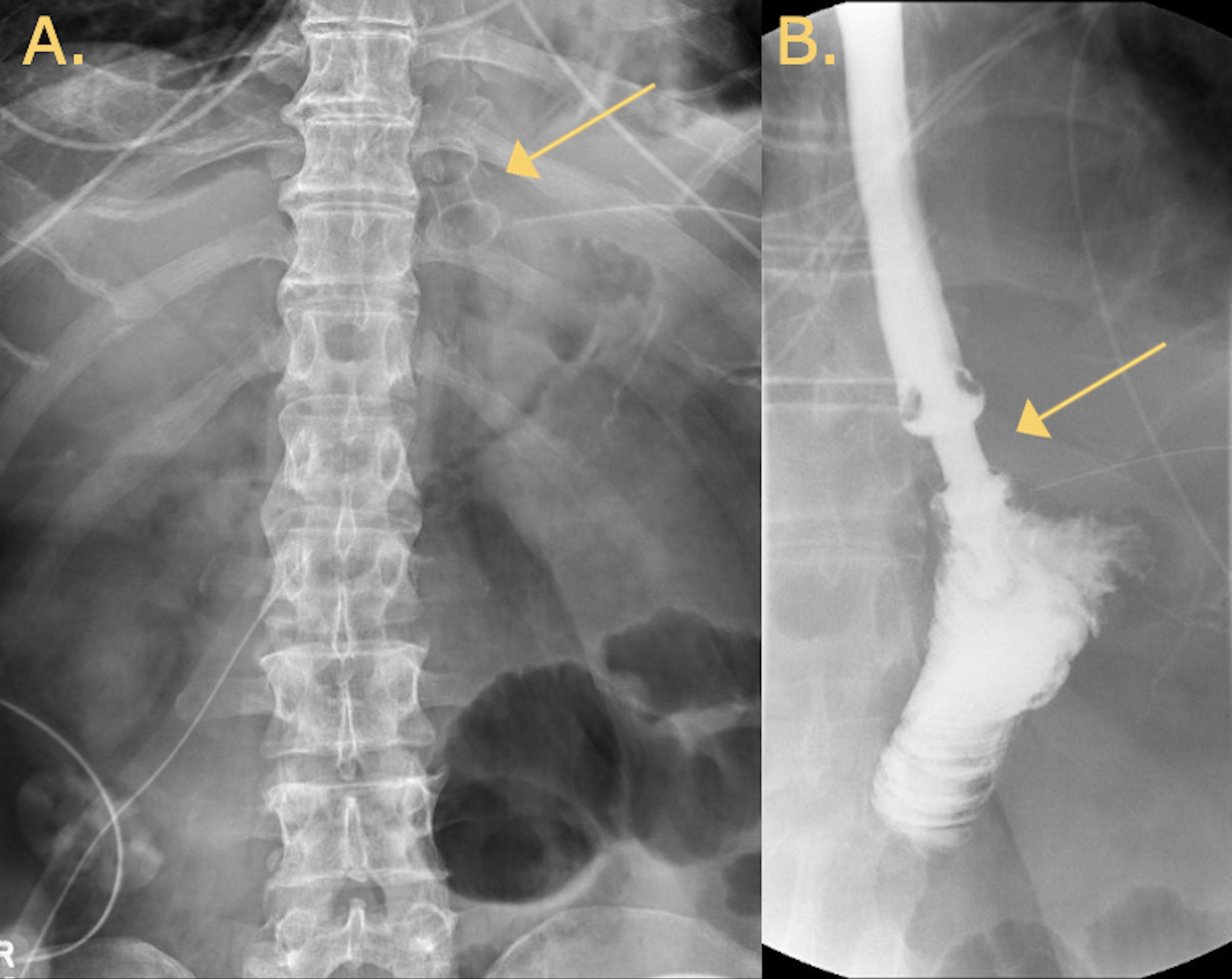
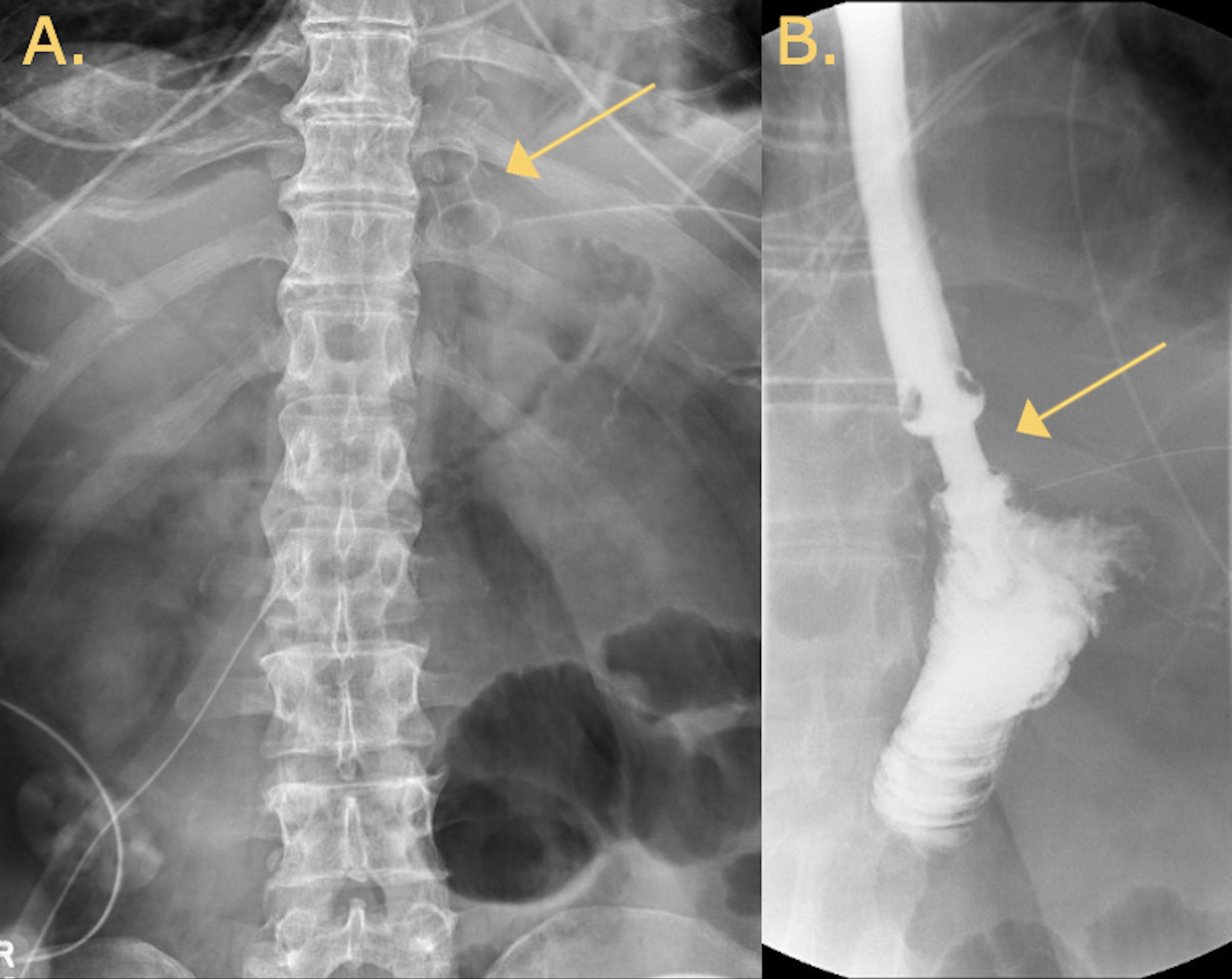
Figure: A: Abdominal x-ray two days post esophagojejunal anastomosis procedure showing stent in place.
B: Upper GI study with gastrografin two days post esophagojejunal anastomosis procedure showing stent in place and no evidence of extravasation.
B: Upper GI study with gastrografin two days post esophagojejunal anastomosis procedure showing stent in place and no evidence of extravasation.
Disclosures:
Abby Kunitsky indicated no relevant financial relationships.
Steve Siegal indicated no relevant financial relationships.
Mark Bloomston indicated no relevant financial relationships.
Bassan Allan: Springworks Therapeutics – Speaker.
Augustine Salami indicated no relevant financial relationships.
Abby Kunitsky, DO1, Steve Siegal, MD2, Mark Bloomston, MD3, Bassan Allan, MD3, Augustine Salami, MD4. P1122 - Endoscopic Ultrasound-Guided Esophagojejunal Anastomosis: A Case Series on the Novel Technique and Our Experience, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.


