Sunday Poster Session
Category: Liver
P1131 - Disparities in Chemotherapy and Radiation Therapy for Hepatocellular Carcinoma: The Impact of Race and Socioeconomic Status
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
- MG
Mahi Gangavarapu, BA
University of Missouri - Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Praneet Khanna, BA1, Samuel J. Kim, BA1, Mahi Gangavarapu, BA1, Tayla Miller, MS2, Bianca Ituarte, BA3, Islam Mohamed, MD2
1University of Missouri-Kansas City School of Medicine, Kansas City, MO; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3University of Missouri - Kansas City, Kansas City, MO
Introduction: Hepatocellular carcinoma (HCC) is a major cause of cancer mortality. Disparities in healthcare access and outcomes persist among different racial and socioeconomic groups. This study investigates how race and income interplay with other demographics to influence receiving chemotherapy and radiation therapy for the treatment of HCC.
Methods: Demographic and clinical data of patients with microscopically confirmed HCC were extracted from the Surveillance Epidemiology and End Results (SEER) database, including variables such as race, median household income, age, sex, rural/urban status, and treatment modalities (chemotherapy and radiation therapy). Chi-square tests, Cox proportional hazards models, and Poisson regression were used for analysis.
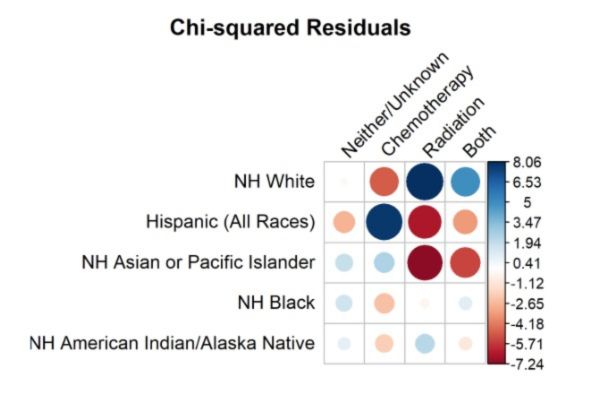
Results: There were significant racial and socioeconomic disparities in HCC treatment and outcomes. Non-Hispanic (NH) White patients were more likely to receive radiation therapy, while Hispanic patients were more likely to receive chemotherapy. NH Asian or Pacific Islander (API) patients were the least likely to receive either treatment (p=0.839). Patients with higher incomes were more likely to receive both therapies (p=0.010). NH White patients had a 33% lower risk of death with chemotherapy and a 28% lower risk with radiation when compared to no treatment. Other racial groups showed significant benefit only from radiation, with a 35% lower risk of death (p=0.002). Combined treatments (chemotherapy + radiation) decreased the risk of death by 21% for Non-Hispanic White patients. Additionally, higher-income patients had a 12% lower risk of death (p=0.001). Hispanic patients had a 22% longer delay to treatment, NH Black patients had a 4% longer delay, and NH American Indian/Alaska Native patients had a 25% longer delay in comparison to NH White. NH API experienced a 4% shorter time to treatment in comparison to NH White. Urban patients experienced a 10% longer time to treatment than their rural counterparts.
Discussion: This study highlights significant disparities in chemotherapy and radiation therapy received and effectiveness among HCC patients, which may be influenced by race and median household income. Non-Hispanic White patients and those with higher incomes are more likely to receive these treatments, which are associated with improved survival outcomes. Targeted interventions are needed to address these disparities and ensure equitable cancer care and patient outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Praneet Khanna, BA1, Samuel J. Kim, BA1, Mahi Gangavarapu, BA1, Tayla Miller, MS2, Bianca Ituarte, BA3, Islam Mohamed, MD2. P1131 - Disparities in Chemotherapy and Radiation Therapy for Hepatocellular Carcinoma: The Impact of Race and Socioeconomic Status, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Missouri-Kansas City School of Medicine, Kansas City, MO; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3University of Missouri - Kansas City, Kansas City, MO
Introduction: Hepatocellular carcinoma (HCC) is a major cause of cancer mortality. Disparities in healthcare access and outcomes persist among different racial and socioeconomic groups. This study investigates how race and income interplay with other demographics to influence receiving chemotherapy and radiation therapy for the treatment of HCC.
Methods: Demographic and clinical data of patients with microscopically confirmed HCC were extracted from the Surveillance Epidemiology and End Results (SEER) database, including variables such as race, median household income, age, sex, rural/urban status, and treatment modalities (chemotherapy and radiation therapy). Chi-square tests, Cox proportional hazards models, and Poisson regression were used for analysis.
Results: There were significant racial and socioeconomic disparities in HCC treatment and outcomes. Non-Hispanic (NH) White patients were more likely to receive radiation therapy, while Hispanic patients were more likely to receive chemotherapy. NH Asian or Pacific Islander (API) patients were the least likely to receive either treatment (p=0.839). Patients with higher incomes were more likely to receive both therapies (p=0.010). NH White patients had a 33% lower risk of death with chemotherapy and a 28% lower risk with radiation when compared to no treatment. Other racial groups showed significant benefit only from radiation, with a 35% lower risk of death (p=0.002). Combined treatments (chemotherapy + radiation) decreased the risk of death by 21% for Non-Hispanic White patients. Additionally, higher-income patients had a 12% lower risk of death (p=0.001). Hispanic patients had a 22% longer delay to treatment, NH Black patients had a 4% longer delay, and NH American Indian/Alaska Native patients had a 25% longer delay in comparison to NH White. NH API experienced a 4% shorter time to treatment in comparison to NH White. Urban patients experienced a 10% longer time to treatment than their rural counterparts.
Discussion: This study highlights significant disparities in chemotherapy and radiation therapy received and effectiveness among HCC patients, which may be influenced by race and median household income. Non-Hispanic White patients and those with higher incomes are more likely to receive these treatments, which are associated with improved survival outcomes. Targeted interventions are needed to address these disparities and ensure equitable cancer care and patient outcomes.
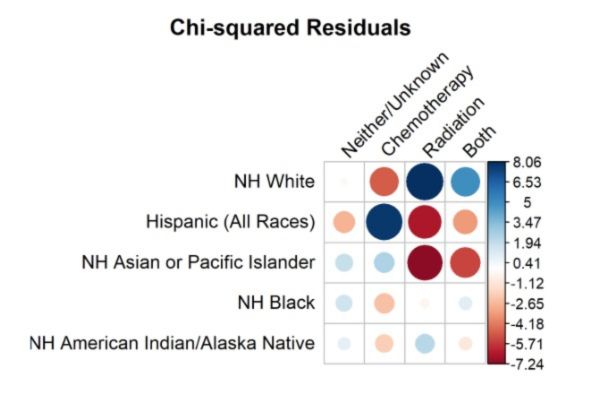
Figure: Chi-Squared Residuals by Race and Treatment Modality in Hepatocellular Carcinoma:
Figure 1 displays the chi-squared residuals for different racial groups and their likelihood of receiving various treatment modalities (neither/unknown, chemotherapy, radiation, both) for hepatocellular carcinoma.
Figure 1 displays the chi-squared residuals for different racial groups and their likelihood of receiving various treatment modalities (neither/unknown, chemotherapy, radiation, both) for hepatocellular carcinoma.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Praneet Khanna indicated no relevant financial relationships.
Samuel Kim indicated no relevant financial relationships.
Mahi Gangavarapu indicated no relevant financial relationships.
Tayla Miller indicated no relevant financial relationships.
Bianca Ituarte indicated no relevant financial relationships.
Islam Mohamed indicated no relevant financial relationships.
Praneet Khanna, BA1, Samuel J. Kim, BA1, Mahi Gangavarapu, BA1, Tayla Miller, MS2, Bianca Ituarte, BA3, Islam Mohamed, MD2. P1131 - Disparities in Chemotherapy and Radiation Therapy for Hepatocellular Carcinoma: The Impact of Race and Socioeconomic Status, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

