Sunday Poster Session
Category: Liver
P1186 - Palliative Care Utilization Patterns in Hepatocholangiocarcinoma
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Malik Salman, BS
Creighton University School of Medicine
Omaha, NE
Presenting Author(s)
Malik Salman, BS1, Xinxin Wu, BS, BA1, Mohammed Al Kurnas, BS, MS1, Peter T. Silberstein, BS, MD2
1Creighton University School of Medicine, Omaha, NE; 2Creighton University Medical Center, Omaha, NE
Introduction: Hepatocholangiocarcinoma (HCC) is a rare primary liver cancer that has features of both hepatocellular carcinoma and cholangiocarcinoma. Due to the aggressive nature of the malignancy, it carries a poor prognosis with a 5-year mortality rate of 79%. Improvements in quality of life, physical, and emotional distress have been linked to palliative care utilization in liver disease. There has yet to be a study analyzing disparities in the demographic factors of patients with HCC receiving palliative care.
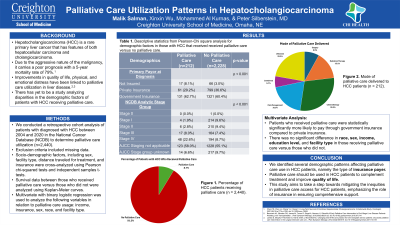
Methods: We conducted a retrospective study of patients diagnosed with HCC utilizing the National Cancer Database (NCDB) from 2004 to 2020 (n=2,449). The usage and type of palliative care were cross-analyzed with demographics including sex, facility type, distance traveled for treatment, and insurance, using Pearson chi-squared tests and independent samples t-tests. Survival data between those who received palliative care versus those who did not were analyzed using Kaplan-Meier curves. Multivariate with binary logistic regression was used to analyze the following variables in relation to palliative care usage: income, insurance, sex, race, and facility type. Exclusion criteria included any missing data.
Results: Of 2440 patients diagnosed with HCC, 9% received palliative care, while 91% did not. 67% of patients who received palliative care were male, while 34% were female. Patients with poorly differentiated HCC were more likely to receive palliative care than those with moderately differentiated cancer (24% vs 9%, P< 0.05). Patients were more likely to receive palliative care in pain management form than surgery for symptomatic alleviation (19% vs 8%, P< 0.05). Of patients who received palliative care, there was no significant difference in age at diagnosis or great circle distance. Patients who received palliative care were significantly more likely to pay through government insurance compared to private insurance (61% vs 36%, P< 0.05 CI = 0.22 - 0.67). Patients who received palliative care had a survival time of 9.1 months, compared to 46.6 months in those who did not (P< 0.05).
Discussion: We identified several demographic patterns affecting palliative care use in HCC patients, namely the type of insurance payer. Palliative care should be used in HCC patients to complement treatment and improve quality of life. This study aims to take a step towards mitigating the inequities in palliative care access for HCC patients, emphasizing the role of insurance in ensuring comprehensive support.
Disclosures:
Malik Salman, BS1, Xinxin Wu, BS, BA1, Mohammed Al Kurnas, BS, MS1, Peter T. Silberstein, BS, MD2. P1186 - Palliative Care Utilization Patterns in Hepatocholangiocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Creighton University School of Medicine, Omaha, NE; 2Creighton University Medical Center, Omaha, NE
Introduction: Hepatocholangiocarcinoma (HCC) is a rare primary liver cancer that has features of both hepatocellular carcinoma and cholangiocarcinoma. Due to the aggressive nature of the malignancy, it carries a poor prognosis with a 5-year mortality rate of 79%. Improvements in quality of life, physical, and emotional distress have been linked to palliative care utilization in liver disease. There has yet to be a study analyzing disparities in the demographic factors of patients with HCC receiving palliative care.
Methods: We conducted a retrospective study of patients diagnosed with HCC utilizing the National Cancer Database (NCDB) from 2004 to 2020 (n=2,449). The usage and type of palliative care were cross-analyzed with demographics including sex, facility type, distance traveled for treatment, and insurance, using Pearson chi-squared tests and independent samples t-tests. Survival data between those who received palliative care versus those who did not were analyzed using Kaplan-Meier curves. Multivariate with binary logistic regression was used to analyze the following variables in relation to palliative care usage: income, insurance, sex, race, and facility type. Exclusion criteria included any missing data.
Results: Of 2440 patients diagnosed with HCC, 9% received palliative care, while 91% did not. 67% of patients who received palliative care were male, while 34% were female. Patients with poorly differentiated HCC were more likely to receive palliative care than those with moderately differentiated cancer (24% vs 9%, P< 0.05). Patients were more likely to receive palliative care in pain management form than surgery for symptomatic alleviation (19% vs 8%, P< 0.05). Of patients who received palliative care, there was no significant difference in age at diagnosis or great circle distance. Patients who received palliative care were significantly more likely to pay through government insurance compared to private insurance (61% vs 36%, P< 0.05 CI = 0.22 - 0.67). Patients who received palliative care had a survival time of 9.1 months, compared to 46.6 months in those who did not (P< 0.05).
Discussion: We identified several demographic patterns affecting palliative care use in HCC patients, namely the type of insurance payer. Palliative care should be used in HCC patients to complement treatment and improve quality of life. This study aims to take a step towards mitigating the inequities in palliative care access for HCC patients, emphasizing the role of insurance in ensuring comprehensive support.
Disclosures:
Malik Salman indicated no relevant financial relationships.
Xinxin Wu indicated no relevant financial relationships.
Mohammed Al Kurnas indicated no relevant financial relationships.
Peter Silberstein indicated no relevant financial relationships.
Malik Salman, BS1, Xinxin Wu, BS, BA1, Mohammed Al Kurnas, BS, MS1, Peter T. Silberstein, BS, MD2. P1186 - Palliative Care Utilization Patterns in Hepatocholangiocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
