Sunday Poster Session
Category: Liver
P1219 - Virtual Reality Application in Hospitalized Patients With Decompensated Cirrhosis: A Feasibility Pilot Study
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio

Kathryn A. Schmidt, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Kathryn A. Schmidt, MD, Alberto Alberto Calleri, MD, Kamalpreet S. Hara, MBBS, Xiao Jing (Iris) Wang, MD, Douglas Simonetto, MD
Mayo Clinic, Rochester, MN
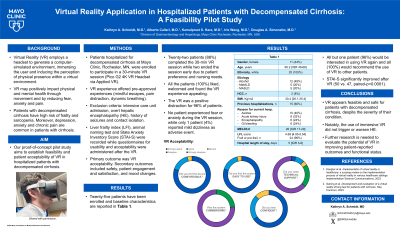
Introduction: Virtual reality (VR) applications are increasingly common, offering enhanced engagement, and gamification. VR may positively impact physical and mental health through movement and by reducing fear, anxiety and pain. Our proof-of-concept pilot study aims to establish feasibility and patient acceptability of VR in hospitalized patients with decompensated cirrhosis.
Methods: Patients hospitalized for decompensated cirrhosis at Mayo Clinic, Rochester, MN, were enrolled to participate in a 30-minute VR session (Pico G2 4K VR Headset via Applied VR) with pre-approved experiences (mindful escapes, pain distraction, dynamic breathing). Exclusion criteria were: intensive care unit admission, overt hepatic encephalopathy (HE), history of seizures and contact isolation. Liver frailty index (LFI), animal naming test and State Anxiety Inventory Score (STAI-S) were recorded while questionnaires for usability and acceptability were administered after the VR. Primary outcome was VR acceptability. Secondary outcomes included safety, patient engagement and satisfaction, and mood changes.
Results: Ten patients have been currently enrolled [20% female; median age 66 years (range 45-77); all white]. The etiology of cirrhosis was alcohol-related in 40%, MASLD in 20%, MET-ALD in 30%, and other in 10%, with a median MELD3.0 score of 28. All patients had history of decompensating events (100% ascites, 40% HE) requiring prior hospitalizations in 60% of cases. Median LFI score was 5.2 (78% frail). Eighty percent of patients completed the single 30-minute VR session, while two ended the session early due to patient preference and nursing needs. No adverse events were reported. No worsening or new HE was recorded. The baseline STAI-S didn’t change significantly after the VR experience (46 and 49 points, respectively; paired-p=0.1). All patients found the VR easy to use and felt confident using it. Additionally, 100% found VR to be a positive distraction, and 90% felt very engaged during the experience, while no one experienced anxiety, pain, or fear.
Discussion: VR appears feasible and safe for patients with decompensated cirrhosis, despite the severity of their condition. Notably, the use of immersive VR did not trigger or worsen HE. All patients enjoyed and welcomed the VR experience, finding it to be a positive distraction. Further research is needed to evaluate the potential of VR in improving patient-reported outcomes as well as functional status.
Disclosures:
Kathryn A. Schmidt, MD, Alberto Alberto Calleri, MD, Kamalpreet S. Hara, MBBS, Xiao Jing (Iris) Wang, MD, Douglas Simonetto, MD. P1219 - Virtual Reality Application in Hospitalized Patients With Decompensated Cirrhosis: A Feasibility Pilot Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Virtual reality (VR) applications are increasingly common, offering enhanced engagement, and gamification. VR may positively impact physical and mental health through movement and by reducing fear, anxiety and pain. Our proof-of-concept pilot study aims to establish feasibility and patient acceptability of VR in hospitalized patients with decompensated cirrhosis.
Methods: Patients hospitalized for decompensated cirrhosis at Mayo Clinic, Rochester, MN, were enrolled to participate in a 30-minute VR session (Pico G2 4K VR Headset via Applied VR) with pre-approved experiences (mindful escapes, pain distraction, dynamic breathing). Exclusion criteria were: intensive care unit admission, overt hepatic encephalopathy (HE), history of seizures and contact isolation. Liver frailty index (LFI), animal naming test and State Anxiety Inventory Score (STAI-S) were recorded while questionnaires for usability and acceptability were administered after the VR. Primary outcome was VR acceptability. Secondary outcomes included safety, patient engagement and satisfaction, and mood changes.
Results: Ten patients have been currently enrolled [20% female; median age 66 years (range 45-77); all white]. The etiology of cirrhosis was alcohol-related in 40%, MASLD in 20%, MET-ALD in 30%, and other in 10%, with a median MELD3.0 score of 28. All patients had history of decompensating events (100% ascites, 40% HE) requiring prior hospitalizations in 60% of cases. Median LFI score was 5.2 (78% frail). Eighty percent of patients completed the single 30-minute VR session, while two ended the session early due to patient preference and nursing needs. No adverse events were reported. No worsening or new HE was recorded. The baseline STAI-S didn’t change significantly after the VR experience (46 and 49 points, respectively; paired-p=0.1). All patients found the VR easy to use and felt confident using it. Additionally, 100% found VR to be a positive distraction, and 90% felt very engaged during the experience, while no one experienced anxiety, pain, or fear.
Discussion: VR appears feasible and safe for patients with decompensated cirrhosis, despite the severity of their condition. Notably, the use of immersive VR did not trigger or worsen HE. All patients enjoyed and welcomed the VR experience, finding it to be a positive distraction. Further research is needed to evaluate the potential of VR in improving patient-reported outcomes as well as functional status.
Disclosures:
Kathryn Schmidt indicated no relevant financial relationships.
Alberto Alberto Calleri indicated no relevant financial relationships.
Kamalpreet S. Hara indicated no relevant financial relationships.
Xiao Jing (Iris) Wang indicated no relevant financial relationships.
Douglas Simonetto: BioVie – Consultant. Mallinckrodt – Consultant. Resolution Therapeutics – Consultant.
Kathryn A. Schmidt, MD, Alberto Alberto Calleri, MD, Kamalpreet S. Hara, MBBS, Xiao Jing (Iris) Wang, MD, Douglas Simonetto, MD. P1219 - Virtual Reality Application in Hospitalized Patients With Decompensated Cirrhosis: A Feasibility Pilot Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
