Sunday Poster Session
Category: Liver
P1246 - Prior Overt Hepatic Encephalopathy and Diagnosis of Minimal HE Significantly Adds to Risk Prediction for MELD3.0 in Patients With Cirrhosis
Sunday, October 27, 2024
3:30 PM - 7:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Kevin V. Houston, MD
Virginia Commonwealth University Health System
Glen Allen, VA
Presenting Author(s)
Kevin V. Houston, MD1, Andrew Fagan, BS2, Gowthami Kanagalingam, MD3, Leroy R. Thacker, PhD3, Jasmohan S.. Bajaj, MD4
1Virginia Commonwealth University Health System, Glen Allen, VA; 2Hunter Holmes McGuire VA Medical Center, Richmond, VA; 3Virginia Commonwealth University Health System, Richmond, VA; 4Virginia Commonwealth University and Central Virginia Veterans Healthcare System, Richmond, VA
Introduction: Despite being a major burden on patients (pts) and families, hepatic encephalopathy (HE) is not included in liver transplant (LT) prioritization. With MELD3.0 there are questions regarding HE as a contributor towards poor outcomes. Cognitive testing for minimal HE (MHE) diagnosis & prior HE hospitalizations could add objectivity. Aim: Define contribution of HE (prior HE & MHE) towards death, LT & future HE independent of MELD3.0.
Methods: We analyzed pts with cirrhosis who had undergone MHE testing using PHES (psychometric hepatic encephalopathy score) from 2002-2023 at a LT center. Prior HE, MELD3.0 at time of testing, comorbidities, medications, & cirrhosis severity were assessed. All pts were followed until death, LT, or last follow-up. Intervening HE-related hospitalizations were also evaluated. Time to events were recorded and Cox proportional hazards analysis with C-statistics were performed for MELD3.0 alone versus MELD3.0 plus other clinical variables.
Results: 609 pts (61±8.4 yrs, 95% men, 66% White) with MELD3.0 (15.0±9.0) were included; pts had alcohol etiology 129 (21%), prior HE 230 (38%), varices 226 (37%), betablockers 198 (33%), depression 122 (20%) and anxiety in 59 (10%). MHE was diagnosed in 333 (55%) pts. Outcomes showed follow-up of 27.7±34.1 months, 252 (41%) died, 147 (24%) received LT, 93 (15%) developed HE & 379 (62%) were hospitalized.
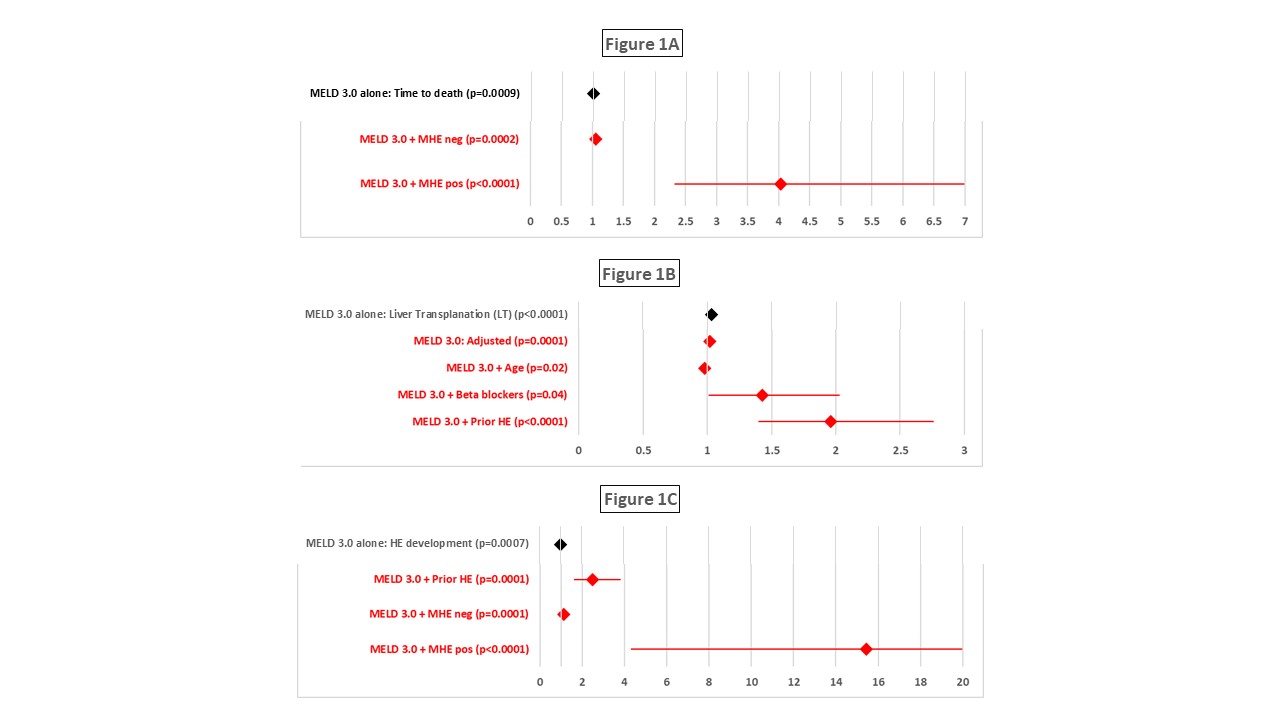
Prior HE pts were more likely to have advanced cirrhosis, including MHE (Table 1) and had a greater likelihood of death, LT, & HE episodes. MHE positive pts were more likely to die and develop HE, but did not affect LT. Prior HE and MHE status were significantly associated with outcomes independent of MELD3.0 (Figure 2). Significant interactions between MHE and MELD3.0 with higher contribution towards LT and death in pts with MHE and higher MELD3.0 were found. There was an increase in Harrell’s Concordance statistic to predict time to death from MELD3.0 alone (0.67) to 0.69 with the additional factors. Similarly, factors added to the C-statistic for LT (MELD3.0 0.69 to 0.74). HE prediction was increased beyond MELD3.0 (C-statistic 0.73) to 0.79 with the remaining variables.
Discussion: MHE diagnosed using PHES and prior HE strict definitions added significantly to MELD3.0 in prediction of time to death, LT, and HE episodes in >600 pts with cirrhosis. There was a significant interaction between MHE status and MELD3.0 for prediction of outcomes and testing for MHE could improve risk stratification.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kevin V. Houston, MD1, Andrew Fagan, BS2, Gowthami Kanagalingam, MD3, Leroy R. Thacker, PhD3, Jasmohan S.. Bajaj, MD4. P1246 - Prior Overt Hepatic Encephalopathy and Diagnosis of Minimal HE Significantly Adds to Risk Prediction for MELD3.0 in Patients With Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Virginia Commonwealth University Health System, Glen Allen, VA; 2Hunter Holmes McGuire VA Medical Center, Richmond, VA; 3Virginia Commonwealth University Health System, Richmond, VA; 4Virginia Commonwealth University and Central Virginia Veterans Healthcare System, Richmond, VA
Introduction: Despite being a major burden on patients (pts) and families, hepatic encephalopathy (HE) is not included in liver transplant (LT) prioritization. With MELD3.0 there are questions regarding HE as a contributor towards poor outcomes. Cognitive testing for minimal HE (MHE) diagnosis & prior HE hospitalizations could add objectivity. Aim: Define contribution of HE (prior HE & MHE) towards death, LT & future HE independent of MELD3.0.
Methods: We analyzed pts with cirrhosis who had undergone MHE testing using PHES (psychometric hepatic encephalopathy score) from 2002-2023 at a LT center. Prior HE, MELD3.0 at time of testing, comorbidities, medications, & cirrhosis severity were assessed. All pts were followed until death, LT, or last follow-up. Intervening HE-related hospitalizations were also evaluated. Time to events were recorded and Cox proportional hazards analysis with C-statistics were performed for MELD3.0 alone versus MELD3.0 plus other clinical variables.
Results: 609 pts (61±8.4 yrs, 95% men, 66% White) with MELD3.0 (15.0±9.0) were included; pts had alcohol etiology 129 (21%), prior HE 230 (38%), varices 226 (37%), betablockers 198 (33%), depression 122 (20%) and anxiety in 59 (10%). MHE was diagnosed in 333 (55%) pts. Outcomes showed follow-up of 27.7±34.1 months, 252 (41%) died, 147 (24%) received LT, 93 (15%) developed HE & 379 (62%) were hospitalized.
Prior HE pts were more likely to have advanced cirrhosis, including MHE (Table 1) and had a greater likelihood of death, LT, & HE episodes. MHE positive pts were more likely to die and develop HE, but did not affect LT. Prior HE and MHE status were significantly associated with outcomes independent of MELD3.0 (Figure 2). Significant interactions between MHE and MELD3.0 with higher contribution towards LT and death in pts with MHE and higher MELD3.0 were found. There was an increase in Harrell’s Concordance statistic to predict time to death from MELD3.0 alone (0.67) to 0.69 with the additional factors. Similarly, factors added to the C-statistic for LT (MELD3.0 0.69 to 0.74). HE prediction was increased beyond MELD3.0 (C-statistic 0.73) to 0.79 with the remaining variables.
Discussion: MHE diagnosed using PHES and prior HE strict definitions added significantly to MELD3.0 in prediction of time to death, LT, and HE episodes in >600 pts with cirrhosis. There was a significant interaction between MHE status and MELD3.0 for prediction of outcomes and testing for MHE could improve risk stratification.
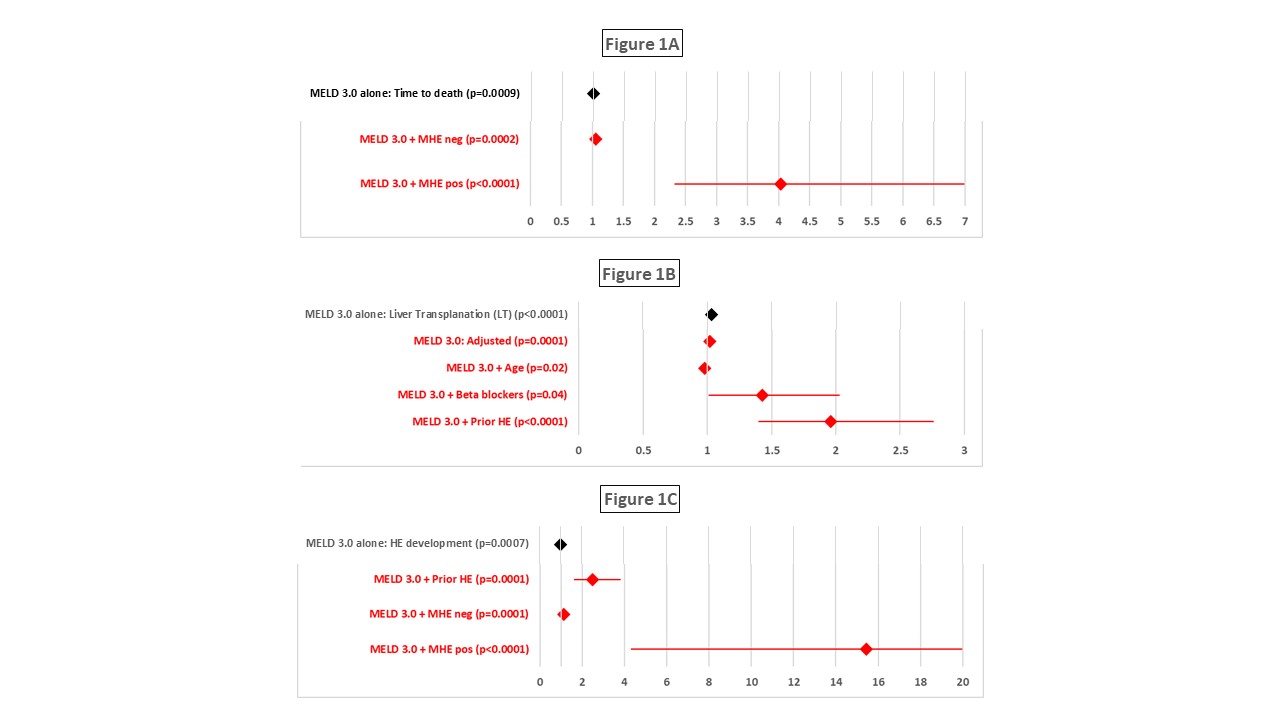
Figure: Outcomes for Death (1A), Liver Transplant (1B), and Hepatic Encephalopathy (1C) are depicted with adjusted Cox Proportional Hazards. Calculation with MELD3.0 alone is depicted in black color. MELD3.0 adjusted for additional factors is also shown in red color.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Kevin Houston indicated no relevant financial relationships.
Andrew Fagan indicated no relevant financial relationships.
Gowthami Kanagalingam indicated no relevant financial relationships.
Leroy Thacker indicated no relevant financial relationships.
Jasmohan Bajaj: Salix Pharmaceuticals – Clinical Trial Investigator.
Kevin V. Houston, MD1, Andrew Fagan, BS2, Gowthami Kanagalingam, MD3, Leroy R. Thacker, PhD3, Jasmohan S.. Bajaj, MD4. P1246 - Prior Overt Hepatic Encephalopathy and Diagnosis of Minimal HE Significantly Adds to Risk Prediction for MELD3.0 in Patients With Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
